Coronary Artery Calcification and Coronary CTA:
Clinical:
Basis for coronary calcium screening:
The lifetime risk of developing coronary
artery disease (CAD) after 40 y of age is 49% for men and 32%
for women [123]. Cardiovascular disease is the leading
cause of mortality for both men and women [259]. Of the
300-450,000 annual events of sudden cardiac death in the US,
nearly 40% of them can be attributed to previously unrecognized
CAD [123]. Pre-clinical detection of CAD can result in early
institution of risk modification. Assessment for the presence of
coronary artery calcium is an excellent method for screening
asymptomatic patients for the presence of CAD.
Atherosclerosis is a complex pathologic process characterized by lipoprotein deposition, a maladaptive inflammatory response, ensuring apoptosis and necrosis, and healing with calcification and fibrosis [264]. Therefore, the development of atherosclerotic plaque is accompanied by the deposition of crystals of hydroxyapatite (calcium phosphate) [45] and calcification does not occur in normal coronary arteries. Hence, the presence of coronary artery calcification (CAC) indicates underlying coronary artery disease [9] and the amount of calcification correlates with the atherosclerotic plaque burden [24,45,83,100]. In one study, 35% of patients with a calcium score between 11-400 had significant coronary stenoses on CTA, and this increased to 65% of patients with a score above 400 [83]. More importantly, 21-47% of patients with normal myocardial perfusion exams have extensive CAC (>400) and this can result in risk reclassification (to high risk) and more aggressive medical therapy [196]. In one study, of asymptomatic patients with normal MPI exams, up to 54% of patients were reclassified as high risk based upon calcium scores of greater than 100 [236]. In another study of patients with normal PET/CT perfusion exams, 30% had calcium scores ≥ 100 and of patients considered low risk by FRS, 57% had evidence of subclinical CAD based upon the presence of CAC [197]. Despite normal perfusion exams, patients with high calcium scores have been shown to be at increased risk for coronary events [197].
Who to screen?:
Unfortunately, clinical risk factors do not always identify
patients with atherosclerotic CAD [28]. The best use of CAC
screening is to refine patient cardiac event risk assessment by
providing incremental information over conventional risk factors
[45,46]. The Framingham risk score
(FRS) has been used to stratify patients risk for developing
coronary artery disease and their 10 year risk
[169]. The score considers traditional risk factors for
CAD including age, gender, diabetes, systolic blood pressure,
total cholesterol, HDL cholesterol, and smoking history to predict
the patients 10-year risk for hard CAD
events [169,222]. A person with a likelihood of cardiac events of
less than 6-10% per 10 years is considered low risk and is
unlikely to benefit from additional cardiac testing [92,222]. An
intermediate risk FRS is associated with 6-19% ten year risk for a coronary event, and a high FRS
has a greater than 20% risk [222]. Unfortunately, up to 20% of CAD
events can occur in patients without major risk factors [169] and
CAC has been shown to outperform FRS for overall risk
stratification [198]. As the Framingham risk score identifies
short term risk only, a more appropriate measure of cardiovascular
risk may be an overall lifetime risk assessment [288].
Idenitification of younger individuals with low-short term, but
high lifetime risk identifies a group of patients that would
benefit from earlier lifestyle modification [289]. Present
guidelines recommend the calculation of lifetime cardiovascular
risk for all individuals between the ages of 20-39 years and for
those between the ages of 40-59 years in the non-high Framingham
risk category [288]. Unfortunately, even among young patients with
low short and lifetime risks, up to 15% have at least a moderate
degreee of coronary atherosclerosis (as denoted by a CAC > 100)
[289].
For patients in the intermediate FRS risk category (or for patients with 3 or more cardiac risk factors) coronary artery calcium scoring can provide incremental prognostic information regarding risk prediction for coronary events [28,29,195] and is cost effective in this population (which comprises about 40% of the general population [92]) [45]. After CAC screening, as many as one-half of patients originally classified as Framingham intermediate risk, are reclassified to high risk or low risk [264]. For intermediate FRS patients, a calcium score of under 100 places them into a lower risk category (annual CHD death or MI rate of 0.4%), compared to an annual CHD death or MI rate of 2.4% if their score is greater than 400 [127]. In one study [195], 16% of intermediate risk patients were reclassified as high risk following CAC screening [195]. SPECT MPI is insufficient to identify the coronary atherosclerotic burden or to reveal coronary stenoses lacking hemodynamic significance [237]. Even in patients with normal myocardial perfusion exams, up to 17.5% can be shown to have coronary artery disease with calcium scores of greater than 100 [57]. Early identification of these patients can result in earlier medical intervention and risk factor modification [57]. The American College of Cardiology/American Heart Association Expert Consensus Document recommends that CAC screening can be considered in asymptomatic subjects with an intermediate risk (FRS 10-20%) [224,228].
High risk patients probably do not require CAC screening for risk
assessment [195]. Even if classified as low risk based upon CAC
screening, high risk patients have been found to have a higher
coronary event rate [195]. Patients with chest pain that is
typical of angina should be evaluated with MPI or coronary CTA
[236].
CAC screening in diabetes:
Patients with diabetes have a 4 times greater incidence of CAD than the general population [80] and CAD is the leading cause of death in diabetic patients- accounting for 75% of deaths [222]. CAD is commonly silent in patients with diabetes and when CAD becomes clinically manifest in diabetics it is often in an advanced state [80,222,282,301]. Silent ischemic coronary artery disease can be found in 6-59% (up to 75% of patients aged 65 years or older [222]) of diabetics [68,119,207,282] and approximately 20-40% of asymptomatic diabetic patients have abnormal myocardial perfusion studies [123,140]. (Other authors indicate that abnormal perfusion exams can be found in 21-59% of asymptomatic diabetic patients, with 15-20% of patients having high risk findings [222]). However, recent studies have suggested that SPECT-MPI screening in asymptomatic diabetic patients does not lead to improvement in cardiac outcomes- likely due to implementation of aggressive medical therapy in these patients [183,184]. Even diabetic patients with a normal myocardial perfusion exam can have annual cardiac event rates of 3-6%, which is more than twice that of nondiabetic patients with a normal stress exam [202]. [229]. Asymptomatic diabetic patients can also have abnormal perfusion exams even in the absence of stenotic coronary lesions and this is felt to be secondary to impairment in endolethial vasodilatation in small coronary vessels [229].
Early CAC screening of asymptomatic diabetes may prove beneficial [68]. An Agatston score > 0 can be found in up to 43% of asymptomatic diabetics under the age of 40 years [287]. CAC measurements can provide additional risk stratification for asymptomatic diabetic patients (diabetics with calcified coronary plaques are 4 times more likely to experience a cardiac event than persons without diabetes with low Agatstons scores [287]) [183] and there is an increasing event-rate with increasing CAC-risk category [301]. In general, diabetics have higher CAC scores compared to patients without diabetes (the likelihood of having a CAC score in the highest age/gender quartile is 70% greater for diabetics) [68]. Additionally, for every increase in CAC score, there is a greater increase in the mortality rate for diabetic patients than for patients without diabetes [68,220]. Measurements of CAC have been found to be superior to established cardiovascular risk factors (Framington Risk Score) in predicting silent myocardial ischemia and short term cardiovascular events in asymptomatic diabetic patients [119,183]. Importantly, diabetic with low CAC scores (<10) have a favorable prognosis- with an annual event rate as low as 0.2% [183,202,301]. Berman et al. suggest SPECT-MPI for diabetic patients with CAC scores above 400 [183], while other authors suggest MPI if the CAC score is above 100 [222].
A multimodality approach to the identification of CAD in diabetic patients may prove to be the most useful [140]. Despite abnormal SPECT imaging, up to 30% of asymptomatic diabetic patients may show no evidence of coronary artery calcifications (frequently due to the presence of non-calcified plaque, although microvascular disease and endothelial dysfunction can also produce perfusion abnormalities in these patients) [140].
Coronary CTA imaging can also be used for the assessment of CAD in diabetic patients [301]. In one study, 41% of plaques in diabetics were non-calcified and would not have been appreciated on CAC-CT [162,229] and up to 70% of asymptomatic diabetic patients with normal SPECT imaging can show evidence of coronary artery disease at CT coronary angiography (both obstructive and non-obstructive) [140]. In studies comparing asymptomatic diabetic and non-diabetic patients using CCTA the prevalence of coronary plaques ranged from 80-93% (significant stenosis 29-33%) in diabetic patients compared to the control population (range 7-16%) [162]. In another study of asymptomatic diabetic patients, coronary CTA revealed a high prevalence of CAD (85% of patients) which was mostly non-obstructive (51%), but obstructive CAD (50-70% stenosis) was found in 27% of patients and severe CAD (>70% stenosis) in 7% [301]. An increase in event rate was observed with increasing coronary stenosis severity [301]. In this same group of patients, a negative CTA exam was associated with a very good prognosis (event rate 3% over an 8 year period) [301]. However, coronary CTA screening may not provide survival benefit in asymptomatic high risk diabetic patients compared to optimal medical treatment [301].
CAC screening in end-stage renal disease:
The risk for adverse cardiac events rises significantly once the eGFR falls below 60mL/min/m2 [206]. Patients with end-stage renal disease (ESRD) also have a higher incidence of CAD- in fact, CAD is the leading cause of death (43-50%) in patients with ESRD and this typically occurs within the first year of hemodialysis [70,177]. Chronic kidney disease patients have a more than 10 to 20 fold increased risk of cardiac death compared to age and gender-matched control subjects without chronic kidney disease [152,206]. Patients with ESRD that receive some form of dialysis have a 100-fold higher risk of death from cardiovascular disease than matched healthy controls [123]. More importantly, a large percentage of patients on hemodialysis with significant coronary artery disease are asymptomatic [206]. In one study of patients with ESRD, 70% of the patients had calcium scores above the 75th percentile for gender- and aged-matched population without ESRD [230]. In a prospective study of asymptomatic ESRD patients undergoing hemodialysis, significant coronary artery narrowing (over 75%) was present in 71% of patients [123]. Additionally, the administration of drugs that influence cardiovascular function such as dipyridamole or adenosine may elicit a significant reduction in blood pressure or heart rate in dialysis patients because their autonomic function is impaired [152]. Diabetic patients with chronic kidney disease have an even higher cardiac event rate compared to nondiabetic patients with chronic renal disease [206]. The early detection and treatment of coronary artery disease in patients with end-stage renal disease may result in improved outcomes [70].
CAC screening in patients with prior XRT:
CAC screening prior to planned coronary intervention:Patients that have received prior radiation therapy to the mediastinum (such as lymphoma patients) have been shown to be at an increased risk for premature coronary artery disease (especially patients that have received more than 30 Gy) [133]. Asymptomatic coronary artery disease can be found in 21-89% of lymphoma patients that had received XRT to the mediastinum and a significant number can have stenoses over 50% [133]. Both coronary artery calcium scoring and coronary CT angiography may play a role in evaluating these patients [133]. A significant number of patients have been shown to have calcium scores above the 90th percentile for their age and sex [133].
CAC can be performed prior to planned PCI to aid in lesion characterization [307]. Severely calcified plaques present a challenge for PCI as they typically result in smaller final lumen diameter and less lumen gain following stenting compared with non-calcified lesions [307]. Additionally, there is a lower procedural success rate, a more frequent rate of acute complications (such as dissection), and a greater propensity for restenosis [307]. The AHA guidelines indicate that rotablation is reasonable for fibrotic or heavily calcified plaque lesions [307]. A pre-lesion calcium score >/= 453 can predict the need for rotablation with a sensitivity of 93% and specificity of 88% [307].
Both the prevalence of CAD and mortality associated with it
appear to be increased among HIV patients [242]. HAART is
independently associatedwith a 26% relative increase in the rate
of MI per year of exposure [242].
Family history of CAD in a first-degree relative is also a risk
factor for premature CAD- the younger the age of CAD onset in the
relative, the higher the risk to the other first degree relatives
[244].
Significance of exam findings:
For both helical and EBCT, an Agatston scoring scale is
used to quantify the amount of calcium identified.
CT calcium scoring is a strong predictor of cardiovascular risk,
independent of clinical risk factors or the Framingham risk score
[264]. In asymptomatic patients a negative CT test makes the
presence of atherosclerotic plaque very unlikely and is associated
with a low risk for a cardiovascular event in the next 2-5 years
(and perhaps even out to 10-12 years [235]) [35]. The ability of a
zero CAC score to exclude CAD is highly dependent on the pre-test
likelihood of CAD [312]. The reported event rate for a zero CAC
score in asymptomatic patients is 0.1-0.5 % per year (the event
rate for patients with normal MPI exams is 0.6-1% per year)
[236,237,274]. The 10 year risk is approximately 1% for patients
without CAC, which is well below the traditional low risk
threshold of <6-10% 10 year risk [274]. Additionally, the
negative predictive value of a CAC score of zero is higher than
the NPV of exercise testing [281]. It is important to remember
that the prognostic implications of a CAC score of zero are less
reliable in symptomatic patients as atherosclerosis can still
occur in the absence of CT-detectable calcification [237,270].
Although SYMPTOMATIC patients without CAC have a significantly
lower event rate than those with CAC (1.8% versus 9%), the event
rate is still higher than that among asymptomatic patients [271].
Among symptomatic
patients with a CAC score of 0, up to 13% can be shown to have
non-obstructive CAD and up to 3.5% can have obstructive CAD
(stenosis > 50%) by CCTA [270]. Other authors quote higher
rates of obstructive CAD in symptomatic patients with CAC scores
of zero, and therefore, absence of CAC in symptomatic patients
cannot reliably exclude important CAD [271]. However, when
symptomatic patients are stratified according to clinical risk
(low or intermediate risk, as opposed to high risk), the absence
of CAC may carry adequate negative predictive value [271,281].
Addtionally, the presence of CAC in symptomatic patients with
nonobstructive CAD is associated with an increased hazard for
death or MI [294]. The overall mortality risk in these patients is
proportional to the coronary calcium score (mortality was 1.5% at
4 years for a score of 1-10, but 10.4% for a score of equal to or
greater than 400) [294].
Conversely, patients with CAC have an adjusted relative risk
ratio for cardiac events 20 times higher than that for patients
without CAC [29]. In general, the higher the calcium score, the
greater the risk for cardiac events [130,174]- in one study, the
risk of cardiac death or non-fatal MI was 3.9 times higher for
patients with calcium scores greater than 300, compare to patients
with a calcium score of zero [28]. Another study found that a CACS
greater than 300 was associated with a hazard ratio for future
coronary heart disease events of nearly 10 [195]. The annual risk
of death from a cardiovascular event or MI has been reported to be
less than 0.4% for patients with no CAC, 1.3% for a score between
100-399, and ≥ 2% for patients with scores greater than 400
[174,193]. In another study of asymptomatic patients, the hazards
ratio for major CAD events (compared to patients with a score of
zero) was 5.3 for a score of 1-100, 10.8 for a score of 101-300,
and 12.0 for a score greater than 300 [271]. Studies have shown
that increasing calcified plaque continues to predict a graded
decrease in survival even with extensive Agatston scores of over
1000, with no apparent upper threshold [291]. Importantly, even
minor amounts of CAC are associated with increased risk for
cardiovascular events- in the MESA study, investigators noted a
threefold relative increase in hazards ratio for those with a
score of 1-10 compared to those with a score of zero [283].
Studies have also shown that the severity of coronary artery
stenosis and frequency of myocardial infarction/events correlate
with the amount of calcification [9,10,30,35].
Current
evidence
supports
aggressive
anti-atherosclerosis
therapy
in
patients
with
calcium
scores
above 100 [46]. Interestingly, patients who are given the results
of their CAC score are more likely to modify their CAD risk
factors and lower their LDL-cholesterol [235].
The presence of even moderate amounts of coronary calcium on CT (scores over 100) have been shown to be associated with silent ischemia in up to 18% of patients [45] and can predict an increased risk for cardiac events in symptomatic and asymptomatic individuals [24]. In an EBCT study, silent myocardial ischemia was found in 2.6% of patients with a score between 11 and 100, 11.3% of patients with a score between 101 and 399, and 46% of patients with a score above 400 [282]. The ACC foundation/AHA expert consensus document reported a summary relative risk ration of 4.3 for any detectable calcium when compared with a calcium score of 0 and raising up to more than 10 in patients with extremely severe coronary calcification [170]. However, at what calcium score should further cardiac evaluation be performed? Although coronary artery calcification is indicative of atherosclerotic plaque disease, it is not specific for luminal obstruction [127]. Among patients reported in the literature, coronary artery scoring resulted in positive findings in 78% of patients, but has been associated with inducible ischemia in only about one-fifth of patients [170]. Other authors indicate that 56% of patients with with scores greater than 100 have normal myocardial perfusion imaging [207].
Because CAC has only a poor to modest correlation with the degree
of coronary lumenal stenosis, myocardial perfusion imaging should
be considered in patients with high CAC scores to better define
the clinical significance of the patients underlying coronary
artery disease [45,271]. Despite the lack of a strong site-to-site
correlation between calcification and lumenal stenosis, the CAC
score gives a close approximation of the total atherosclerotic
burden [271]. In general, the likelihood for the rpesence of
iscehmia on myocardial perfusion SPECT exam (MPS) increases with
increasing calcium score [83,100,283] and there appears to be a
direct relationship of the extent and severity of perfusion
abnormalities to the CAC score [95]. The frequency for ischemia on
perfusion imaging is most common in patients with scores above 400
[283] and scores above 400 have also been shown to be associated
with decreased coronary flow reserve [310]. Calcium scores between
100-399 represent an intermediate risk group [311]. However, for
patients with scores between 100 and 400, the frequency of
inducible ischemia is higher in patients with diabetes and/or
metabolic syndrome (13% versus 4%) [283,311].
|
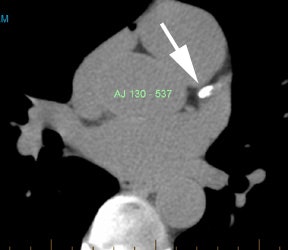
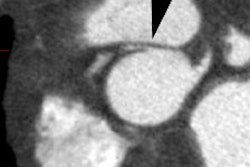
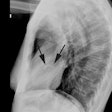
Coronary artery calcification: The patient below has a large calcification in their proximal LAD. Their total calcium score was 537. |
|
|
CAC can aid in further patient risk stratification- for patients with low- and intermediate risk, a low calcium score is associated with an event rate below that predicted by the Framingham criteria alone [134]. A study comparing the FRC score to CAC evaluation (with CT angiography) found that the presence of any CAC was 97-98% sensitive for the presence of CAD [198]. In fact, if subjects were excluded from further screening because of a low risk FRC score, almost 2/3's of women and 25% of men with substantial atherosclerosis would have been missed [198]. In intermediate risk patients, the use of coronary calcium scoring can result in reclassification of more than half of the patients (16-22% reclassified as high risk, and 30-39% reclassified as low risk) [220]. The negative likelihood ratio (which is the factor by which a negative test result reduces the odds of having a disease) is excellent for CAC scoring and superior to that of the FRC score [198]. For example- assigning a woman to the low-risk Framingham risk category decreases her odds of having moderate or greater plaque burden by just 29%, whereas the absence of calcium decreases her odds by 96% [198]. Conversely, in a prospective study, intermediate FRS individuals with CAC scores > 300 had an annualized hard cardiac event rate of 2.5% (absolute 10 year risk > 20%) and would have therefore been re-classified into the high-risk group following the results of CAC imaging [207]. Overall, in intermediate risk patients, the use of coronary calcium scoring can result in reclassification of more than half of the patients (16-22% reclassified as high risk, and 30-39% reclassified as low risk) [220].
Coronary artery calcification also carries prognostic information as the greater the amount of calcification identified- the more likely the patient is to have a cardiac event [4,10]. When the CAC score is combined with data from a myocardial perfusion exam there is improved risk stratification, incremental prognostic information is obtained, diagnosis is improved, and there is improved patient management [179,236,237,308]. A CAC score of 400 or more is suggestive of advanced coronary artery disease and an increased risk for hard cardiac and cardiovascular events (even scores between 100-399 have an increased risk for hard cardiac and cardiovascular events [285]) [264,285]. Even for patients with normal perfusion scans, although the short term risk has been shown to be low, the long term relative risk for total cardiac and all-cause death/MI events significantly increases when the coronary artery calcium score is greater than 400 [284,308]. In one study of subjects with a normal MPI exam, a CAC score > 400 was associated with a 3.55 fold increased risk for any cardiac event (and 2.75 fold increased risk for cardiac death/MI) compared to patients with minimal CAC (less than 10) [236]. In fact, a CAC score of >400 with normal MPI results was associated with an approximately 3% annual event rate [236]. In another study of patients with normal MPI, 78% had a CAC greater than zero, 56% had a score greater than 100, and 31% had a score greater than 400 [237]. The annualized event rate for patients with calcium scores greater than 400 can be as high as 14% [11].
Additionally, in patients with significant coronary artery stenoses, the presence of CAC is associated with a worse prognosis [1]. Clinical decisions should not be based solely on the coronary artery calcium score [5]. Other factors such as individual risk factors and medical history need to be reviewed [5].
The extent of calcification has a high correlation with a
significant stenosis somewhere in the involved coronary
vessel and the greater the extent of calcification, the more
severely narrowed the coronary artery is likely to be [4]. In
general, the extent of calcification also affects the likelihood
for an abnormal MPI exam. In one study, 41% of asymptomatic
patients with a calcium score of greater than 400 had abnormal
MPS, whereas, no abnormal scans were observed in patients with
scores of under 100 [29]. In another study of asymptomatic
patients, ischemia was identified on perfusion imaging in 27% of
patients with CAC scores above 1000, but in only 1.9% of patients
with scores below 1000 [226]. Myocardial perfusion imaging (MPS)
has been shown to be normal in up to 87% of vessels with calcium
scores of less than 10, and in 85% with scores between 11-100 [83]. For scores between 11-100, MPS will demonstrate
evidence of ischemia in 1.7- 4.8% of patients [95,179]. For scores
between 100-400, MPS will be abnormal
in 5-18% of patients [95,236]. Approximately 25% of patients with
a score of greater than 400 will have abnormal MPI exams [236].
Generally, patients with a calcium score of greater than 400 are
considered to be at the greatest increased risk for subsequent
cardiac events [31]. These data help to support the notion of CAC
as a gatekeeper for MPI imaging [236]. It is generally accepted
that further diagnostic imaging is not required in asymptomatic
patients with a CAC score below 100 [237]. Using a cut-off of
100-400 would decrease MPI utilization by 42% (a cutoff of over
400 would decrease MPI usage by 69%) [236]. However, this cutoff
may not apply to high-risk patients such as diabetics [237]. In a
prospective evaluation of asymptomatic diabetic patients, 18.4% of
patients with scores between 11-100 had perfusion abnormalities on
SPECT imaging [237].
In general, the prevalence of abnormal MPS is between 15-46% for
patients with calcium scores over 400 [45,95,179].
These
results
indicate
that
the
likelihood
of
myocardial
ischemia
by
SPECT
is
related to the coronary calcium score [46] and that it is
appropriate to evaluate asymptomatic patients with CAC scores
above 400 using MPS [95]. Another study demonstrated that when
used in combination with a SRS (summed rest score) of at least 2
or a SSS (summed stress score) greater than 8, a CAC score of
greater than 400 identified patients at highest risk for severe
cardiac events [179]. Bear in mind that many patients with scores
above 400 still have normal MPS exams [83]. Importantly, data
suggests that when patients with high CAC scores have normal MPS
findings, their prognosis with aggressive medical treatment is
good [45] with an annualized event rate as low as 1% [119,207].
Although a CAC score of 400 is a reasonable threshold to prompt
MPS in patients with a low to intermediate likelihood for CAD, an
important point to consider is that patients with a high clinical
likelihood for CAD may require a lower CAC score threshold [106].
In patients with multiple CAD risk factors, MPS can be considered
in symptomatic patients and even those with low calcium scores as
up to 15% of patients with scores of less than 100 may have
perfusion abnormalities on MPS [74]. Therefore, CAC screening and
myocardial perfusion imaging should be considered complimentary
examinations and should be used in conjunction with the patients
clinical evaluation to determine the most appropriate management
[45,74,106]. The appropriate use
criteria for cardiac radionuclide imaging state that MPI is
appropriate in asymptomatic patients who are high risk for CAD (by
ATP III criteria), high CHD risk patients with a CACV of 100-400,
and in patients with a CAC > 400 at any CHD risk level [236].
Unfortunately, a single standard score to define abnormal is unlikely to be applicable to all ages and both sexes [5]. Although the actual calcium score is a good indicator of overall extent of disease, it may not be as useful for predicting cardiac events as a percentile ranking [24]. This is because coronary artery calcium generally increases with age [24,127]. A calcium score above the 75th percentile for age and sex matched individuals is associated with a much greater risk for cardiac events compared to individuals in the 25th precentile [24]. For instance, a calcium score of 40 in a 40 year old man would place him above the 95th percentile, while a 70 year old man with an identical score would be below the 10th percentile [24]. Patients in the top calcium score quartile have up to an 8-fold increased risk for cardiac events compared to patients in the lowest quartile [45]. Patients with a score greater than the 75th percentile for age and gender should be considered to undergo intensive risk factor modification and lipid-lowering therapy [127]. Asymptomatic patients with calcium scores above 100 who are above the 90th percentile should also be considered for SPECT myocardial perfusion evaluation due to their increased frequency of silent ischemia [46]. However, although a high percentile ranking is indicative of long-term risk for cardiac events, the finding is not always associated with ischemia on perfusion imaging [77]. In fact, there is a low likelihood (2.5-7%) for identification of ischemia on perfusion imaging in patients with scores below 100 due to the sub-clinical level of atherosclerotic disease [77]. Hence, perfusion imaging may not be required if the calcium score is less than 100, despite a high percentile ranking [77]. This group of patients (high percentile score with CAC less than 100), however, can benefit from aggressive antiatherosclerotic intervention [77].
|
Calcium Score |
Recommendation |
|
Less than 100 (but high
percentile) |
Does not necessarily
require perfusion imaging (MPS). (+) Atherosclerotic
intervention. |
|
Percentile 90% or higher and
score over 100 |
MPS should be performed |
|
Over 400 |
MPS should be performed |
|
Score 100-399 |
Consider clinical
factors: sex, chest pain sx's, diabetes and selective
MPS evaluation |
|
|
|
Other authors suggest that a vessel-specific calcium score is actually superior and more accurately reflects the presence of coronary artery disease compared to whole-heart Agatston scoring [217].
Of course, coronary calcium score is just another variable to
consider when evaluating a patient. Gender, smoking, and the
presence of symptoms may modify a patients overall risk for
cardiac events and the need for further cardiac evaluation [45].
Patients with chest pain and
symptomatic patients:
The American College of Cardiology/American Heart Association has
endorsed the use of CAC scoring as a filter before invasive
coronary angiography or hospital admission for patient with chest
pain symptoms, especially those with symptoms atypical for cardiac
ischemia [271]. A finding of a CAC score of zero in a low risk
patient presenting with chest pain, an equivocol ECG, and negative
enzymes has a sufficient near term favorable prognosis that the
patient can be safely discharged without further testing
[271,274].
Articles are suggesting that even in symptomatic patients, a
negative calcium score carries prognostic significance. In a
meta-analysis of the use of CAC screening in symptomatic patients,
only 2% of patients with a CAC score of zero had a >50%
stenosis on ICA [276]. In the CONFIRM study of symptomatic
patients predominantly with an intermediate probability of CAD,
the prevalence of a stenosis≥ 50% with a CAC score of zero was
3.5% (and 82% of these patients had single vessel disease) [276].
However, other studies have suggested variable rates of
obstructive CAD ranging from 8-19% [276]. This variability exists
because the probability of CAD is driven in large part by the
clinical pre-test probability for CAD [276]. Risk factors
associated with a higher likelihood for CAD despite a negative CAC
scan include patients presenting with typical angina, smoking, and
a family history of premature CAD [276].
Even if coronary artery disease is present, a score of zero in a
symptomatic patient is still associated with a favorable near-term
prognosis, particularly in patients in the low-to-intermediate
risk category [276]. In the same meta-analysis, only 1.8% of
patients with no evidence of coronary calcium had a cardiovascular
event in comparison to 9% of patients with detectable calcium
[276]. In the CONFIRM study, there was no difference in all-cause
mortality in patients without coronary calcium despite the
presence of of nonobstructive ot obstructive CAD [276].
Some authors have suugested that in low risk symptomatic patients
referred for coronary CTA, a negative CAC score is associated with
an excellent prognosis and that CTA imaging may not be necessary
[276].
Pre-operative evaluation:
The presence of CAC on pre-operative CT scanning is associated
with cardiac complications during non-cardiac thoracic surgery,
however, the positive predictive value is low (23%). The absence
of coronary artery calcium has been shown to be a reliable
predictor of a favorable post-op cardiac course [3,265]. Coronary
artery calcium scoring can aid in further patient risk
stratification following pre-operative myocardial perfusion
imaging evaluation [265]. Patients with normal pre-operative MPI
exams, but high calcium scores (over 1314) have an increased risk
for perioperative cardiac events (12% versus 5%) [265]. The
highest rate of perioperative cardiac events was observed in
patients with abnormal MPI and high calcium scores (22%) [265].
Limitations:
Despite a strong correlation between the CAC score and the
severity of CAD, the CAC score itself cannot differentiate between
obstructive and non-obstructive CAD [312]. Additionally, coronary
calcium scoring cannot rule out coronary artery disease in all
patients [77]. In asymptomatic patients, a calcium score of zero
indicates a very low likelihood for significant/obstructive
coronary artery disease (prevalence of
obstructive CAD is lower than 1% [281]), however, it does
not completely exclude the risk for cardiac events [28]. Critical
single vessel CAD can occur in 2-5% of subjects with a negative
CAC score [45], but the likelihood for obstructive CAD depends
strongly on the population that is being studied and may be less
useful in symptomatic patients [281,312].
Approximately 5% of patients with acute myocardial infarction have no coronary artery calcium [77]. Although a recent prospective study found no evidence of flow-limiting CAD in stable symptomtic patients with low- or intermediate risk factors [281], several studies have reported that up to 8.7% of symptomatic patients with zero or low calcium scores can have obstructive coronary artery disease (≥ 50%) [210]. Other studies have noted that in symptomatic patients, between 1-39% will have obstructive CAD on angiography, despite a calcium score of zero [221,281]. In patients presenting with suspected ACS, up to 39% of the culprit lesions will have no evidence of calcification [221]. These findings suggest that calcification reflects chronic, stable CAD and may not be the best method to evaluate symptomatic patients [221].
Middle-aged women with a smoking history appear to be particularly susceptible to having events in the absence of, or with minimal CAC [45]. In a study in the Journal of the American Medical Association, coronary events were observed in 4.4% of patients with calcium scores of zero during a mean follow-up of 7 years [28]. These events are likely related to rupture of soft, unstable lipid plaques [28,45]. However, calcium may not have been properly detected in all patients as this study employed a standard CT scanner and 6 mm slice thickness [28]. Retrospective cardiac gating, multidetector imaging, and thinner slices have all been shown to improve detection of coronary artery calcification [8,16,18,27]. CT coronary angiography can be used to detect the presence of soft plaque in symptomatic patients and in patients with a high clinical suspicion, despite negative calcium scores..
Serial Coronary Calcium Evaluation:
Patients with moderately high calcium scores (exceeding 100)
should be treated aggressively with anti-atherosclerosis therapy
[46,56]. Serial monitoring of the
patient's calcium score can be used to assess effectiveness of
medical therapy [46]. Evidence supports that the CAC scores can be
reduced with aggressive lipid-lowering drug therapy (such as
statins which will slow the propagation of vascular calcification)
[46,47]. Treated patients show only a
small progression in calcium score (percent change in volume score
of 10% or less) and can even demonstrate a reduction in the
calcium volume [46]. Conversely, untreated patients can
demonstrate progressive coronary calcification with a 35-40%
increase in calcium volume score [46].
For patients with a negative CAC score on their baseline exam, up
to 36% can have detectable CAC at followup (mean detection
time 6.1 years +/- 3 years) [299]. For patients with an initial
negative exam, a followup study should not be performed sooner
than 4-5 years [237,299]. New-onset CAC at followup most commonly
involves a single vessls (most commonly the LAD) and the calcium
burden is typically low (1-10 in up to 52% of patients, 11-100 in
44% of patients, and >100 in up to 4% of patients) [299].
Patients with initally negative exams at greater risk to develop
CAC on followup include patients with traditional coronary risk
factors such as HTN, DM, smoking, high BMI, and high LDL levels
[299]. Patients with higher baseline scores tend to progress at a
faster rate than individuals with lower baseline scores [46].
Patients that demonstrate progressive coronary calcification with
a change of greater than 30-40% are at high risk for subsequent
myocardial infarction [46]. Asypmtomatic patients with a
significant (>15%) progression of their CAC score on annual
evaluation, have their risk for acute MI increased by 17.2%
compared to patients without progression [264].
X-ray:
The chest radiograph has a low sensitivity for detecting coronary artery calcification. The best site to detect coronary artery calcification on the PA CXR is along the mid left heart border (the left main, and proximal portions of the left anterior descending and left circumflex arteries lie in this location). CAC appears as thin, parallel white lines on the chest radiograph. The accuracy of CXR for detecting coronary calcifications is only 42% [4]. Plain film evidence of coronary artery calcification in symptomatic patients under the age of 65y, is almost always (nearly 100% incidence) associated with significant coronary artery disease. About 30% of asymptomatic patients will also have significant narrowing.
Fluoroscopy has also been used successfully for the
detection of coronary artery calcification. Sensitivity ranges
from 40%-79% [4]. However, up to 48% of calcifications identified
on EBCT can be missed at fluoroscopy [4].
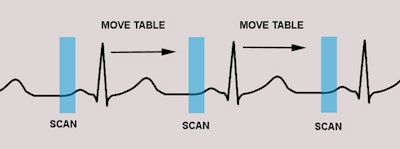
Electron beam CT (EBCT): EBCT was initially used for calcium scoring. EBCT is capable of very rapid scans which can be triggered from prospective ECG gating (generally at 80% of the R-R interval) to minimize cardiac motion [4]. The estimated peak radiation dose from the exam is between 1.1 to 1.3 rad (cGy) and no contrast material is required [4,14]. Overall, EBCT and MDCT have been shown to have equivalent reproducibility for measuring calcium scores [58] and EBCT scanners are no longer produced [271].
Helical CT: For the detection of significant coronary obstructive disease, helical CT has a sensitivity between 88-91% and a specificity of about 50% (accuracy 76%) [4]. The quantity of coronary artery calcifications measured by helical CT correlates positively with obstructive CAD [2] and the absence of coronary calcification has a high negative predictive value for the exclusion of CAD in patients with atypical chest pain [6]. Although lack of calcification does not exclude atherosclerotic plaque (about 5-10% of patients have CAD despite the absence of coronary calcifications) [6] it does indicate a low likelihood for obstructive CAD. Calcific deposits are often blurred on single slice helical imaging because of cardiac and small calcifications may not be seen [4]. Retrospective ECG gating of diastolic data has been shown to improve detection of calcified coronary plaques (less cardiac motion during diastole) [6]. The coronary calcium scoring system used for electron beam CT may not be entirely applicable to helically acquired exams, but further investigation is required [14]. A more appropriate threshold for calcium may be 90 HU [16]. Note however that helical exams are more prone to streak artifacts from calcifications [16]. If these streaks are included when determining the coronary calcium score, the resultant score will erroneously high [16]. The estimated peak radiation dose from the exam is 2.7 rad at the skin (breast dose is 1.8 rad, lung dose 1.7 rad) [14].
Multisection helical CT:
Because of its shorter acquisition time, superior spatial resolution (0.625 mm longitudinal which decreases partial volume artifacts [37]), and temporal resolution approaching that of EBCT, MDCT is superior to EBCT for the evaluation of coronary artery disease [33]. For most patients the mean Agatston score is not significantly changed by using a 1.5 mm reconstruction increment, as opposed to the usual 3 mm increment [88]. The present recommendation is that slices should be reconstructed with 3 mm thickness and that the widest beam collimation that allows reconstruction of 3mm slices should be selected [224]. However, in young patients, very small amounts of calcium may not be identified unless overlapping slice reconstruction is used [88]. In young patients, even small amount of coronary artery calcification can influence the estimation of their cardiovascular risk [88]. (Proposed imaging protocol)
MDCT interscan variability: As with all cardiac calcium
exams, even multi-detector helical CT examinations suffer from
interscan calcium score variability [157]. Generally, variability
is greatest for patients with minimal CAC and decreases with
increasing amounts of CAC. Heart motion (due to limited temporal
resolution) and partial volume averaging can account for a 10-50%
(average about 30%) change in score (depending on lesion size)
when patients are imaged twice within a short interval [24,53]. The percentile ranking assigned to
the two scans can differ in up to 13% of patients (using 4-slice
MDCT), 11-12% for 16-slice scanners, and up to 24% for certain
64-slice scanners (EBCT interscan variability is approximately 15%
(varying from 11-28%)) [42,157]. To reduce interscan variability,
thin slice imaging will help to reduce partial volume effects and
overlapping reconstructions are also useful [53]. When using
prospective gating for the exam, interacquisition variability in
calcium measurements is significantly less at slower heart rates-
likely due to decreased cardiac motion artifacts [21]. One way to
reduce interscan variability is to repeat the exam in subjects who
have a minimal to mild calcium score on the initial scan and
average the two results [22]. Unfortunately, this will increase
patient radiation exposure. The use of calcium volume measurements
rather than a calcium score, has also
been shown to decrease variability in the exam [22]. For a volume
score, all pixels with an identified ROI of 130 HU or more are
included in the score measurement [155]. A recent article has
suggested that among patients with intermediate cardiac risk, the
Agatson score can vary substantially between exams acquired on
different vendors CT scanners [296]. This variability can result
in reclassification of patients to the high- or low-risk
catagories in up to 6.5% of cases [296].
Retrospective ECG gating can be performed to decrease interscan variability and also improve the quality of the exam [35,53]. Using this technique, overlapping MDCT projections with a are continuously acquired and the ECG signal is simultaneously recorded [33]. Algorithms are then used to sort the data from different phases of the cardiac cycle into specific temporal windows (typically 10 windows) based upon the R-wave (i.e.: the R-R interval is divided into 10 equal time windows) [33]. Through the use of retrospective ECG-gating, the point in the cardiac cycle at which cardiac motion is minimal (typically late diastole) is used for image reconstruction producing excellent multiplanar reformatted images [7,13]. Multi-detector exams with retrospective gating have been reported to have less inter-exam variability (to about 10% or less [35,53]) when compared to EBCT studies [18], however, other authors have found persistent high interscan variability [26].
Retrospective ECG gating does not rely on estimation of the presumed next R-R interval as is seen in prospective gating [13]. Reconstruction data intervals can be accurately measured on the basis of the actual R-R intervals that occurred during the scanning [13]. The final reconstruction is based only on images obtained during a portion of mid-diastole, with the reconstruction trigger selected according to the actual heart rate (and this greatly reduces cardiac motion artifacts) [13]. The fastest and easiest image reconstructions use a pre-defined window of 40% of the RCA and 60% for the LAD [26]. However, using preselected reconstruction intervals can result in under-estimation of the true calcium score (and calcium volume)- particularly for patients with mild or moderate amounts of coronary calcium [37]. Improved image quality can be obtained by reconstructing several image sets and selecting the data with the fewest motion artifacts for calcium score determination [26,37]. For multi-detector helical CT acquisitions there is an inverse relationship between heart rate and image quality [13]. Overall, the best image quality is achieved when the patients heart rate is less than 75 beats per minute [13]. Oral beta-blockers before the scan may be considered if the HR is elevated (>75) [224]. Reconstruction image quality decreases with higher heart rates, irregular heart rates, or arrhythmias [13].
Further analysis has shown that each of the individual coronary arteries are best seen at varying points of the cardiac cycle [15]. The LAD at mid-diastole (50-70%), the circumflex at 50-60%, and the right coronary artery at 40-50% [14,15]. The left coronary artery, aortic root, and ascending aorta are best seen at mid-diastole (50-60%) [39]. Detection of small calcifications in the coronary arteries is improved when images are viewed at different reconstruction points [66]. In fact, up to 58% of patients with a calcium score of zero at one reconstruction interval, were found to have coronary artery calcifications when multiple reconstructions were reviewed [66]. The pulmonary arteries are best displayed during mid-to late diastole (80%) [39]. The present recommendation is that the data should be acquired or reconstructed during mid-diastole (70% of the cardiac cycle) [224], however, systolic data may be more appropriate if the HR is greater than 75 [224].
Even with these variations, multidetector CT with retrospective ECG-gating produces cardiac images with fewer motion artifacts and shows a high correlation with coronary artery calcium scores determined using electron beam CT [16].
The one major drawback of retrospective gating is that it
increases the patients radiation exposure compared to prospective
ECG triggering due to oversampling [16]. Present recommendations
suggest the ue of retrospective gating only for patients with
irregular of HR?s above 75 [224]. Radiation dose from
multidetector coronary CT can vary widely depending on the type of
imaging protocol used from 1.5 to 5.2 mSv for male patients, and
from 0.6 to 6.2 mSv for female patients [20,22,23].
The radiation exposure from spiral protocols using retrospective
gating is at least 3 fold higher than that from electron beam CT
[20]. Studies have shown that lower radiation doses can be
used for the exam- this results in images with an increased amount
of noise, but apparently detection of calcification is not greatly
affected [19,23]. A reduced mAs scan based on the patient's BMI
can produce diagnostic quality exams with 40% lower radiation and
does not require changes in the calcium attenuation threshold used
for Agaston score determination (85 mAs for BMI less than or equal
to 30 kg/m2, or 120 mAs for BMI > 30 kg/m2
or weight > 85 kg) [262]. The patient dose can be reduced by
lowering the mAs (to as low as 40-55 mAs) without significantly
compromising exam quality, particularly for non-obese patients [22,60]. The present recommendation is that
the scan should be acquired at 120 kVp [224]. Adjusting the kVp is
not recommended as this can would
require a new Agatston calcium threshold determination for proper
quantification [224,262]. The use of a 100 kVp tube volatage has
been shown to result in an overestimation of the Agatston score
when the standard threshold of 130 HU is used [279,280]. Adjusting
the threshold to 147 HU for 100-kVp exams leads to a better
agreement with standard 120-kVp protocols, but with a persistent
bias towards overestimation [279]- however, other authors suggest
that a simple adjustment in the threshold HU measurement is not
adequate [280].
The current recommendations for CAC imaging are that the radiation dose should average 1.0-1.5 mSv and should not exceed 3.0 mSv (DLP should not exceed approximately 200 mGy x cm) [224].
One other point to consider is that variation in attenuation
values can affect CAC determination (which depends on the
detection of aggregates of contiguous image pixels with
attenuation values greater than 130 HU) [48]. Image attenuation
values have been shown to vary between scanners and by body size
[48]. Absorption of x-rays is higher in obese patients that
results in beam hardening and deviation in the calculated calcium
concentration [237]. This can produce calcium score values that do
not reflect the true calcium burden [48]. Calibration phantoms
containing known amounts of calcium hydroxyapatite and the use of
"fat rings" to simulate a range of patient sizes can improve
accuracy and permit comparability of measurements between persons
imaged on different scanners [48].
The use of adaptive statistical iterative reconstruction to
reduce radiation exposure also results in decreased image noise,
as well as decreased Agatston and calcium volume scores compared
to filtered back projection reconstruction [304]. Use of ASIR can
reduce Agatston score by 10.5-31% [304]. The use of other
iterative reconstruction techniques have not been shown to produce
significant change in calcium score compared to FBP [304].
An Agatston scoring scale is used to determine risk of cardiac events [24]. Using this method the slice thickness should be 3 mm and a Hounsfield density measurement greater than +130 is considered indicative of calcification [4,24]. For each level scanned, all pixels with a HU density measurement greater than 130 HU are then displayed and a region of interest (ROI) is placed around the lesion [9]. If using a more narrow slice thickness, a mathematical correction must be applied to avoid oversampling [24]. For instance, if the slice thickness were 2.5 mm, the appropriate scaling factor would be 2.5/3 [24]. To be considered for the final score determination a calcification needs to have a minimum area of greater 1 mm2 [8] (or three contiguous pixels [127]). Calcifications that do not meet the attenuation threshold (130 HU) or are less than 1 mm2 are not included in the score [155]. A lesion density score is then determined based upon the maximal HU number in each ROI [9]- 1= 130 to 199; 2= 200 to 299; 3= 300-399; and 4 is greater than 400 HU. This lesion density score is then multiplied by the area of each region of interest to determine a calcium score [9]. The total calcium score is determined by adding up each of these scores from each of the four coronary arteries (left main, left anterior descending, circumflex, and right coronary arteries) [9,11]. A total calcium score of 0 is normal; 1-100 considered mild coronary artery disease; 101-400 moderate; and over 401 indicates extensive coronary artery disease and very high risk for cardiac event [30]. Up to 18% of asymptomatic patients with calcium scores between 100-399 will have perfusion abnormalities indicative of ischemia on stress myocardial perfusion SPECT imaging [36]. The higher the coronary artery calcium score, the more likely patients will have an abnormal myocardial perfusion SPECT exam (abnormal scans demonstrating ischemia are found in 45% to 46% of patients with scores above 400) [17,30,36]. Patients with no detectable calcium on EBCT have an excellent prognosis with an annual event rate ranging from 0.06%-0.13% [127].
Scans performed at 3 mm slice thickness are superior to those
performed at 6 mm for accurate determination of coronary artery
calcium score [8]. Even more accurate determinations of calcified
volume can be obtain by using thinner
slices from 0.5-1.5 mm [27,292]. Compared to 3.0mm thick slices,
0.5 mm thick slices can detect coronary artery calcium/subclinical
atherosclerosis in 23% more patients [292]. One drawback of
thinner slices is increased image noise, particularly in patients
with a large BMI [292].
There can be considerable variability in EBCT coronary calcium measurements when two scans are performed on the same patient in close temporal proximity (between 14-50%) [4,5,26]. Interscan variability is most pronounced for patients with low, but non-zero calcium scores [5]. Interscan variation is an important limitation of electron beam CT and patients may require two scans with the higher calcium score used for risk stratification [5]. The interscan variability is likely related to scan misregistration, cardiac motion, breathing, and inherent image noise [4,12,22]. Scanning the entire heart during one breath hold will resolve the problem of scan misregistration [12].
Interscan variabilities can also be decreased by the use of an ECG trigger of 40% of the R-R interval (rather than 80% which is the trigger used for many EBCT exams) [12]. This is because coronary artery motion is at its nadir during early diastole (the period of 30-50% of the R-R interval), while the 80% trigger occurs on or near the P-wave during atrial systole [12]. Images obtained at the end of systole or at early diastole (beginning at 10-30% of the cardiac cycle) also suffer from motion artifact [13]. For prospective triggering of EBCT, the next R-R interval is estimated on the basis of the median of the last seven R-R intervals [13]. Prospective ECG triggering fails with rapid changes in heart rate, as in the case of patients with cardiac arrhythmias [13].
The sensitivity of electron beam CT for coronary artery disease has been reported to be between 88-100% [16] and the overall specificity is about 50%. The low specificity is due to the fact that CAC confirms the presence of plaque disease, but it may not be hemodynamically significant. Absence of CAC implies the absence of a significant coronary artery narrowing and is associated with a very low risk for future cardiac events (annual event rate less than 1%) [4,11]. The negative predictive value of an normal EBCT exam for significant stenosis (ie: 50% or greater) is between 90-95% [4]. However, lack of CAC does not confirm the absence of coronary artery disease- particularly in younger patients [4]. EBCT can be used in the evaluation of patients presenting to the emergency department with chest pain and non-diagnostic ECG's (excluding patients with prior MI or revascularization procedure) [11]. If the patient has a normal EBCT exam the risk of immediate MI is very low and the patient does not necessarily require admission [11]. Unfortunately, patients without visible calcium may still be experiencing an acute coronary syndrome [84]. In fact, 25-40% of culprit lesions are at sites of endothelial erosion with acute thrombus without underlying calcification [143].
In patients with no measurable coronary calcification at baseline, a followup EBCT score must exceed 11.6 Agastone units to qualify for statistically significant progression [63].
CT coronary
angiography:
Approximately 40-60% of the invasive coronary arteriograms
performed in the United States each year do not demonstrate
obstructive CAD [166,213]. In the interest of sparing health care
resources and limit unnecessary invasive testing, a reliable,
non-invasive tool would be highly desirable for the identification
or exclusion of CAD [166]. Myocardial perfusion imaging has long
been used for the evaluation of patients with suspected CAD-
unfortunately, 10-15% of MPI exams are inconclusive and up to 44%
of patients with left main disease will only demonstrate small
(<10%) or no perfusion defects [213]. A large portion of
myocardial perfusion exams are also falsely positive with up to
59% of patients referred for cardiac catheterization based on an
abnormal SPECT exam are shown to have no obstructive CAD [273].
Although coronary calcium score can aid in the detection of CAD in
asymptomatic patients, stenoses can occur in vessels that do not
contain calcification and it cannot be used to determine if there
is a flow limiting stenosis [49,274]. Furthermmore, although the
presence of coronary artery calcification is a specific indicator
for the presence of coronary artery atherosclerosis, it does not
represent the full burden of plaque (CAC is estimated to represent
approximately only 10-20% of the total atherosclerotic plaque
burden) [155,274]. Additionally, recent studies have indicated
that calcification in plaque is an indicator of stable plaque [62]
and that calcification is found infrequently in ruptured plaque
[105]. For patients with low- and intermediate risk, a low calcium
score is associated with an event rate below that predicted by the
Framingham criteria alone [134,274]. Additionally, in asymptomatic
patients CCTA may not provide incremental prognostic information
above that of CAC scoring- in fact, atherosclerosis detected by
CCTA can lead to an increase in invasive testing [274].
However, high risk patients with low calcium scores have been
shown to have the same risk predicted by the Framingham criteria
and therefore, calcium score imaging does not aid in risk
stratification in these patients [134]. In patients considered at
high risk for coronary artery disease, up to 51% of patients with
normal calcium scores can be shown to have non-calcified plaque on
coronary CTA (note: most patients with normal calcium scores show
only mild disease, but up to 4% can show a moderate to severe
stenosis) [134]. In the CORE 64 trial, 20% of symptomatic patients
without CAC had at least one angiographic stenosis of at least 50%
[274]. In another study, 8.2% of symptomatic patients with no
detectable coronary calcium had a greater than 70% stenosis due to
a non-calcified plaque [151]. In another study, 17% of men, and
25% of women had no detectable calcium, but were found to have
plaque by coronary CTA (although in most of these subjects the
plaque burden was mild and only 2.5% of these patients were found
to have a substantial plaque burden) [198]. In another study of
patients with chest pain, 10% of patients were found to have
obstructive coronary artery disease, however, 39% of patients were
found to have non-obstructive CAD [225]. Risk factors in
asymptomatic patients for having exclusively noncalcified plaque
include younger age, familial history of premature CAD, increased
levels of vascular inflammation, smoking history, and diabetes
[274]. None-the-less, these risk factors are associated with only
a slight increase in the relative risk of events and/or mortality
and the absolute-event rates are minimal in the absence of CAC
(1-2% 10 year risk) [274]. On the other hand, the presence of
plaque can prompt more aggressive medical therapy for these
patients [198]. Still, the ACC/AHA recommends against using CCTA
in asymptomatic patients even if those risk factors are present
[274].
Further risk stratification of symptomatic patients based on their pretest probability of CAD, can aid in the prognostic significance of the CAC score [274]. In symptomatic patients with low and intermediate pretest probability of CAD, a CAC score of zero was associated with the presence of significant CAD in 3.4% and 3.9% of patients, respectively [274]. In another study of symptomatic patients without known coronary artery disease, in those with a CAC score of zero, the presence of a ≥ 50% stenosis was 3.5%, and only 1% had a stenosis ≥ 70% (translating to a negative predictive value for excluding 50% and 70% stenoses of 96% and 99%, respectively) [274]. The actual cardiac event rate in these patients has also been shown to be low. In one study of symptomatic subjects with a low to intermediate risk and no CAC, the event rate was slightly <1% [274]. In the CONFIRM registry, in symptomatic patients with a CAC = 0 and only non-calcified plaque at CCTA, < 0.2% of patients suffered hard events of death or MI at 2.1 years of followup [274]. Based on these studies, some authors have suggested that in symptomatic patients with a low pretest likelihood for CAD and a CAC score of zero, no further cardiac testing would be needed [274]. On the other hand, for symptomatic patients with elevated calcium scores > 400, studies have shown that approximately 90% have significant stenosis (>50%) at invasive angiography (suggesting little role for CCTA in these patients) [274]. And in symptomatic patients with CAC scores between 101-400 (or low risk symptomatic patients with a CAC >400), further evaluation with non-onvasive functional imaging or CCTA has been suggested [274].
Vulnerable plaque: Most acute coronary syndromes arise from plaques that are not hemodynamically significant [151]. Studies have demonstrated that almost 70% of coronary occlusions (leading to myocardial infacrtion) result from thrombosis of lesions with a stenosis of less than 50% [191]. Ideally, it is the non-calcified or vulnerable plaque that would be most useful to identify as these plaques can lead to acute coronary syndrome [123,134]. Vulnerable plaques have a large, hypoxic, metabolically active core containing lipid, oxidized lipid, and inflammatory cells (predominantly macrophages that results in FDG accumulation on PET imaging) [164,238]. Vulnerable lesions have a thin fibrous cap that can be weakened by the secretion of proteolytic enzymes from the inflammatory cells [164]. Conventional angiography provides only information about luminal diameter, it does not provide information regarding plaque composition [62,171]. Two specific characteristics of vulnerable plaque are: 1- about 95% of vulnerable lesions are located in proximal, larger-sized coronary arteries; 2- vulnerable plaques tend to be of low attenuation (< 30 HU); and 3- while vulnerable plaques are not lumen-occluding, it has been shown that they fill more than 50% of the vascular cross-sectional area and the plaque volumes are large due to positive (i.e. outward) vessel remodeling [171,185]. Positive vascular remodeling (PR) has been described as an external vessel diameter of >110% compared to a normal proximal or distal segment [185]. It has been suggested that the presence of positive remodeling, low plaque density (LAP), and spotty calcification have a high positive predictive value for culprit plaques associated with acute coronary syndromes, while the absence of these three characteristics showed a high negative predictive value [171,185,238,264]. The presence of low attenuation plaque and positive vessel remodelling provide additional prognostic information with regards to future coronary events [285]. In one study, the presence of both low attenuation plaque and positive remodeling was associated with a 22% likelihood for an ACS over a 2 year follow-up, compared to < 0.5% in patients with plaques that lacked these features [185]. The greater the remodeling and the larger the plaque area, the higher the likelihood for plaque rupture and an earlier acute event [185]. In another study, the presence of low attenuation plaque and positive remodelling was associated with a hazards ratio for cardiac events (sudden cardiac death, MI, and unstable angina) of 11.2 [285]. There appears to be an increased prevalence of noncalcified low attenuation plaque in women [259]. Patients with nonalcoholic fatty liver disease have also been shown to have a higher incidence of high risk plaque [298].
CT angiography can provide additional insight into the presence
of CAD by permitting visualization of non-calcified plaque and has
been shown to be more accurate than calcium scoring in
demonstrating coronary stenoses [49]. Additionally, due to it's
high negative predictive value, the exam is of great use in
patients with low to intermediate risk factors who present with
atypical chest pain [92]. By
demonstrating normal or
non-obstructive CAD, invasive coronary artery angiography can be
avoided [213]. Multidetector CT (MDCT) offers several other
advantages for coronary artery evaluation- the exam is
non-invasive, it can be completed in a short period of time,
myocardial bridging can be readily appreciated, and it can
effectively define coronary anomalies [46,54].
MDCT coronary angiography may also be cost effective- with overall
lower health care costs compared to patients that undergo
myocardial perfusion SPECT imaging and coronary catheterization
[144,182,189,199]. MDCT can also be performed for evaluation of
stenosis of coronary artery bypass grafts [85]. Noncardiac
findings can be seen in 25-61% of patients, of which 5-41% may be
significant or potentially significant [156].
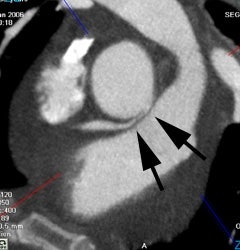
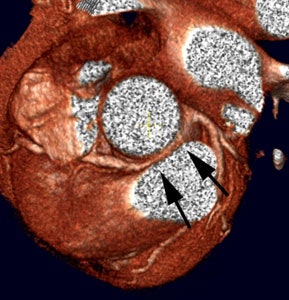
|
Anomalous RCA origin
from the left coronary sinus: The patient below underwent
coronary CT angiography to assess for coronary artery
disease. The patient was found to have an anomalous
RCA arising from the left sinus of valsalva. The
vessel can be seen to course between the pulmonary
trunk and aorta (black arrows) |
|
|
Limitations:
The most significant drawback of the CT exam is in it's suboptimal ability to consistently
detect the presence of anatomic coronary lesions [46]. In general,
visualization of the epicardial coronary arteries is limited by
cardiac motion, the small size of the distal arteries, and the
tortuous course of the vessels through the imaging plane [34,99]. The right coronary artery has the
greatest amount of motion and velocity- generally between 6-42mm
of axial displacement during the cardiac cycle (3-20mm for the
left coronary artery) [99]. Motion artifacts can also be seen in
patients with a pericardial effusion due to a pendulum-like
movement of the heart- the left circumflex and right coronary
arteries are particularly affected [290].
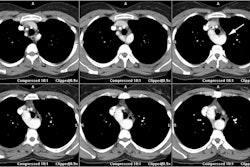
These factors are important because of the limited temporal and spatial resolution of the CT scanner. Temporal resolution is limited to one-half the gantry rotation speed (this is about 200-300 msec for most state of the art scanners) while angiography can capture 30 frames per second (approximately 30 msec temporal resolution). The fastest single-source scanner currently available spins at 270 milliseconds per rotation for a temporal resolution of approximately 135 milliseconds [266]. For motion free evaluation of the coronary arteries the acquisition of the entire heart has to be completed within one diastolic phase [211]. The temporal resolution of a dual head system is approximately one-quarter the gantry rotation time [266]. The fastest dual-head scanner spins at 280 milliseconds per rotation for a temporal resolution of about 70 milliseconds [266]. Therefore, at lower heart rates, the entire heart can be scanned with a dual head system [211]. The spatial resolution is limited by the size of the CT detectors (presently with over sampling the resolution is about 0.5 mm). Therefore, CT coronary angiography generally has very good sensitivity for stenoses in the proximal and mid-segments of the main coronary vessels (vessels over 2 mm in size) [69], but the evaluation of the distal main vessels and their side branches is much more limited [69]. The current generation of 64 slice scanners have an in plane resolution of 0.4 mm, a slice thickness of 0.6 mm, and a temporal resolution of 165 ms [71,75]. Temporal resolution can be improved with:
Multisegment/multicycle reconstruction: For patients with stable and predictable heart rates, the temporal resolution can be further improved to as low as 83 msec by applying a multisegmental reconstruction algorithm [75,99]. With multisegment reconstruction, data of two or more successive cardiac cycles are combined that cover, as separate segments, a 180 degree acquisition [99]. In other words, rather than reconstructing images from a single 180 degree arc during one heartbeat, images are reconstructed from two 90 degree arcs each obtained from a separate heart beat [266]. Because the acquisition of data within each heartbeat is now occurring over a smaller scan angle, the time required for the acquisition is shorter which effectively improves the temporal resolution [266]. The temporal resolution is improved by a factor 2n (n=number of cycles and segments) of the rotation time [99]. Therefore, using a 90 degree arc and two heart beats for data acquisition would rsult in a temporal resolution of about 67 milliseconds (assuming a gantry speed of 270 milliseconds per full roptation) [266]. Multisegment reconstruction requires that the heart must come to rest in the same position with the same cardiac cycle length for every beat of the scan [266]. Otherwise, multisegment reconstruction can result in motion artifact if the heart rate and position are not constant [75,266]. Also- the radiation exposure tends to be higher because of the requirement for overlapping x-ray exposure [266].
Dual Source CT: Dual source CT is characterized by two x-ray tubes and two corresponding detectors mounted on the gantry with an angular offset of 90 degrees [97,99,113]. Thus, a 90 degree rotation of the gantry is sufficient to acquire the 180 degree projection data needed for image reconstruction [113] and this improves the temporal resolution by a factor of 2 [97,99]. With a gantry rotation time of 330 msec, dual source CT has improved temporal resolution (83 msec by half-scan reconstruction- i.e.- one quarter of the gantry rotation time [161]) and this may decrease the need for pharmacologic heart rate modulation [89,97,99]. Second generation dual source scanners have temporal resolutions of 75 millisecondas and a high-pitch spiral scan protocol has been developed that allows scanning of the entire heart with a total scan time of approximately 270 msec [241]. Dual source CT has been shown to have significantly better diagnostic image quality than single source CT - particularly at higher heart rates [161] and has been suggested to have improved accuracy and specificity for the diagnosis of significant stenoses on a per segment basis [180]. Dual source CT may also be useful for the evaluation of patients with atrial fibrillation [109]. Motion free imaging of the coronary vessels is possible even at heart rates of up to 90 bpm [113]. Only heart rates that are both high and variable deteriorate image quality with dual source CT [97,125]. Even cardiac stents may be evaluated without heart rate control [135]. As with single headed CT systems, excessive coronary artery calcification (score >400) will also result in image degradation [125]. Faster gantry rotations are not possible at this time due to an increase in mechanical G-forces that are beyond mechanical engineering limits [99]. For dual source CT, the overall optimal reconstruction window has been suggested to be in late diastole at 65-75% of the R-R interval (for patients with low or intermediate heart rates- under 60 beats per minute) [113,261]. Other authors suggest that the majority of coronary artery segments are evaluable in patients with regular heart rates between 70-110 bpm using a prospectively gated scan with a systolic data aquisition around a center at 40% of the R-R interval [211]. Prospective gated dual source CT results in significant radiation dose reduction to between 2-4 mSv [211]. Overall, in patients with heart rates above 80 bpm, systolic reconstructions may yield superior image quality [113,261]. To achieve optimal image quality in patients with heart rates above 60 beats per minute, systolic and diastolic data may need to be available for review (between 25%-75% of the cardiac cycle) [261]. For patients with low heart rates (sinus rhythm below 60 to 65), a high pitch protocol (pitch 3.4) may be used to images the entire heart during one diastole and significantly reduce radiation dose to about 1.21 mSv (almost a 90% reduction) [211]. The main limitation of high-pitch protocols is that only one data set is acquired [211]. Therefore, no additional reconstructions are possible in case of timing errors, and no functional information can be obtained from the acquisition [211]. However, because the entire heart is scanned within one diastole, there are no step artifacts with this protocol [211].
An increase in body mass index (BMI) results in higher image noise [158,178]. In large patients, an increased bolus dilution due to larger blood volume may also result in a decreased contrast-to-noise ratio and decreased coronary artery attenuation [158,178]. Protocols need to be adjusted to account for BMI in order to improve image quality in larger patients [178].
Another limitation of CT coronary angiography is related to partial volume averaging of coronary artery calcification which results in calcifications appearing larger than their actual size [34].
Finally, it is important to remember that not all coronary stenoses identified by CT are flow limiting lesions [69]. Patient management based solely upon the CT findings can lead to inappropriate revascularization [69]. Myocardial perfusion imaging should be strongly considered in patients with CT lesions to determine their functional significance [69]. Non-flow limiting lesions probably warrant aggressive medical therapy [69].
Contraindications:
1- High density objects: Calcified coronary plaques and metallic cardiac stents can affect the quality of the exam [69]. Coronary artery calcium can negatively impact the ability to evaluate coronary CTA [309]. Dense/large calcifications obscure the true vessel lumen due to blooming effects when the calcification partially extends into adjacent voxels [69]. Therefore, CT angiography may not useful in patients with a heavy burden of calcified plaque (score greater than 400-1000) which precludes adequate evaluation of the degree of stenosis [50,71,276]. Other authors suggest a score of 287 or greater (or 454 if all imaging conditions are optimal) is a value above which more than 50% of cases may not be able to rule out coronary artery stenosis [309]. In an analysis of the CORE-64 trial data, the authors found a significant disagreement between CTA and angiography for the determination of at least 50% coronary stenosis in calcified segments (with decreased specificity in severely calcfied segments-71%, compared to noncalcified segments -99% specificity) [240]. CT has a tendency to overestimate the degree of obstructive CAD in the presence of coronary calcification [240]. Among the segments with false-positive findings at MDCT, 85% had some degree of calcification (mild- 28%, moderate- 29%, and severe- 27%) [240]. However, other authors have found no significant effect in patients with high calcium scores [86]. Also, photon flux through high density objects can sometimes lead to a signal void adjacent to a densely calcified plaque or within a stent which can be misinterpreted as soft plaque [69]. The use of higher spatial frequency algorithms can aid in stent evaluation.
2- Arrhythmias: Patients with atrial fibrillation or other forms of irregular heart rhythms are also not candidates due to the high heart rate variability which results in temporal windows in different cardiac phases and suboptimal image quality [50,102,147]. The timing shift causes spatial inconsistency (typical stairstep appearance) on transverse images and motion artifacts [147]. Patients with mild heart rate irregularities may undergo imaging, but may require ECG editing to improve image quality [67,147]. ECG editing arbitarily modifies the position of the temporal window within the cardiac cycle, but typically requires retrospective data acquisition (which increases patient radiation exposure) [147,268].
3- Patients with breath-hold difficulties and those with the inability to remain supine and motionless are also not likely good candidates for CT coronary imaging [50].
4- Limited diagnostic accuracy has been reported in obese patients with a body mass index of 35 kg/m2 or greater [102].
Other exclusion criteria include known allergy to iodinated contrast, underlying renal dysfunction (serum creatinine greater than 1.36 - 1.5 mg/dL), multiple myeloma, hyperthyroidism, pheochromocytoma, and patients with acute coronary syndromes [52,71].
Patient preparation:
With use of 16 to 64 detector scanners, noninvasive CT imaging of the coronary arteries for non-calcified plaque is done by making adjustments to keep the patients resting heart rate low and utilizing retrospective gated reconstructions [32,33,34]. For coronary CT angiography, image quality is inversely related to the patients heart rate (i.e.: image quality declines with increasing heart rate) [35]. The right and circumflex coronary arteries seem more prone to motion artifact than the LAD- possibly related to their proximity to the atria which is reactivated during early diastole [43]. Motion-free coronary angiograms can be obtained in the majority of patients with heart rates below 80 beats per minute [40], however, the slower the heart rate the better the image quality. Heart rate variability also affects image quality with less variable heart rates producing better quality and more accurate exams [82,132]. This is because the commonly applied relative ECG-gating reconstruction technique (at a certain percentage of the R-R interval) does not generate images in exactly corresponding cardiac phases when there is intercycle variablity in the heart rate [82]. In other words, inconsistencies between heart cycles due to arrhythmia result in merging of slightly different cardiac phases despite acquisition of data from consecutive cardiac cycles at the same percentage in relation to the R wave [132]. With mutisegmented reconstruction techniques, this merging of data introduces blurring of the reconstructed image thereby reducing the number of segments that can be evaluated and decreasing accuracy for stenosis detection [132].
Beta blockade: In general, it is desirable to have the patients heart rate less than 60 (generally between 50-59 bpm). Side effects of β-blockers include hypotension, bradycardia, prolonged AV conduction times, and widened QRS complexes [209]. β-blockers should be used to achieve the desirable heart rate if there are no contraindications (such as asthma, COPD, or bronchospasm on inhalers, sinus bradycardia [HR less than 60 bpm], hypotension [systolic BP less than 100 mmHg], atrioventricular conduction block (second or third degree block), heart failure, diabetes, and Raynaud syndrome) [35,50,72,92]. Caution should be used for patients who are taking other atrioventricular nodal blocking agents such as calcium channel blockers (diltiazem, verapamil), digoxin, and other β-blockers [72].
Oral propranolol (20-40mg) or metoprolol [Lopressor] (50-100mg) given the night before and 1 hour prior to the exam can also reduce heart rate and improve image quality (especially for right coronary artery visualization) [43,50,51]. Metoprolol can also be administered I.V., but requires that patients be monitored (HR and BP) carefully during dosing (the agent has a half-life of 3-4 hours [209]). The initial dose should be 2.5 mg I.V. over one minute [72]. If the heart rate remains above 65 bpm after 5 minutes, an additional dose of 2.5 mg is administered [72]. If the heart rate still remains elevated, up to two additional 5 mg doses can be given (each over one minute) with a 5 minute interval between doses [72]. A total of up to 15 mg of metoprolol can be used I.V. [35,50,72,92]. If the patient has bronchospasm, two puffs of an albuterol inhaler are given [72]. If the patients heart rate drops to less than 45 bpm or develops symptoms due to bradycardia, consideration should given to administer atropine [72]. An initial dose of 0.5-1mg can be given via rapid IV bolus and can be repeated to a maximum dose of 3 mg [209]. If the patient is atropine resistant, resuscitative measures with IV fluids and epinephrine may be required [72]. Symptomatic hypotension can also be treated with IV fluid using 10-20 mL per kg of body weight [209].
Calcium channel blockers can be used to reduce the heart rate in patients with a contraindication to beta-blockers (such as congestive heart failure or asthma) [71,78]. Calcium channel blockers can be administered intravenously [92,297]. Diltiazem is the preferred agent because it shows the least negative inotropic effect [297]. The IV dose of diltiazem is 0.25 mg per kg of body weight up to 25 mg maximum; or in an oral regimen of 30 mg of regular-release diltiazem) [92]. Sublingual administration of short-acting nitroglycerin (1 to 2 tablets equal to 0.4 to 0.8 mg) given immediately prior to scanning has been used to improve visualization of the coronary lumen (via the vasodilatory effect) [71,92,116]. Nitroglycerin has been found to increase proximal coronary artery diameters by 12-21% [99] and allows more septal branches to be visualized [116], but the added value on diagnostic accuracy is not yet clear [99]. Contraindications to nitroglycerin include hypotension, migraine sensitive to nitrates, recent MI, severe anemia, increased intracranial pressure, known hypersensitivity to nitroglycerin, and recent use of nitrate-based medication for erectile dysfunction [92,93].
All patients that receive medication for the exam must be monitored for 30 minutes following the test and must not operate machinery or drive for 3 hours following the IV administration of 10 mg or more of metoprolol [92].
Ivabradine is an agent that is used in certain parts of the world, but it is not yet approved in the US [209]. Ivabradine is a pure heart rate lowering agent that acts by inhibiting the ionic current involved with pacemaker activity in cells of the SA node, with no effect on the duration or morphology of the action potential [209]. The agent reduces the slope of spontaneous diastolic depolarization and lowers heart rate at rest and during exercise- in fact, the agent is rate dependent and has a greater effect at higher heart rates (i.e.- the degree of heart rate reduction increases with increasing heart rate) [209]. As a result, symptomatic bradycardia is rare and the agent can be used in even if patients are taking beta-blockers [209]. Ivabradine has no effect on myocardial contractility or intracardiac conduction and has only minor effects on blood pressure [209]. One study suggested that a 15 mg single dose of the agent or ivabradine 5mg twice daily for 5 days prior to the exam are effective for lowering patient HR [293]. Contraindications to Ivabradine include acute MI, unstable angina, heart failure (functional class II-IV), severe hypotension, sick sinus syndrome or sinoatrial block, 3rd degree AV block, severe hepatic insufficiency, and use of strong cytochrome P450 3A4 inhibitors [209].
Scan Protocol and Radiation Dose:
Generally- scanning should be in a cranial-to-caudal direction- beginning at the carina and extending through the base of the heart during a breath hold [50] Valsalva maneuver should be avoided as this can result in poor contrast enhancement [99]. If bypass grafts or internal mammary arteries are to be evaluated, scanning should begin at the level of the aortic arch [50]. The thinnest detector collimation possible should be used for image acquisition [50]. An initial non-contrast exam is performed to determine the extent of coronary artery calcification which, if severe, will prevent CT angiography [50]. Between 60-120mL of a contrast agent with a high concentration of iodine (300-400 mg/mL) is administered via an 18 to 20-gauge catheter at a rate of 4-6 mL/sec [35,50,71,92,117]. The injection should be followed by a saline flush (25-50 mL at 4-6 mL/s) to decrease beam-hardening artifact within the right ventricle which can obscure the RCA [35,50,71,117]. Alternatively, contrast can be injected in a bi-phasic pattern with 50mL at 4mL/sec and 30-50mL at 2.5 mL/sec followed by a saline flush [51]. Another protocol calls for a biphasic injection with the second phase consisting of a 50 mL mixture of 30% contrast and 70% saline that is then followed by a saline flush [92]. Optimal contrast opacification may require a more sophisticated approach based upon patient body weight as an inverse correlation has been demonstrated between aortic attenuation and body weight [121]. Some authors suggest using 1.0 mL/kg of 350 mg I/mL contrast medium injected at 4.5 mL/s followed by a saline flush [121].
The scan delay can be determined using a test injection (20 mL) with repeated scanning at 2 sec intervals positioned at the level of the aortic root [92]. Scan delayed can be empirically timed to coincide with the beginning of the saline flush (about 25 seconds) or bolus tracking can be performed with an ROI over the ascending aorta [50]. Bolus tracking may yield better vessel enhancement than a test bolus [38]. In general, contrast materials with higher iodine concentrations yield significantly higher attenuation in the coronary arteries [59].
Prospective ECG triggered exam: For prospective ECG gated imaging, the x-ray beam is turned on at predetermined cardiac phases to acquire sufficient data to reconstruct images during the acquisition window [300]. Prospective CT angiography is a step-and-shoot axial (non-helical) examination (effective pitch is 1) with a beam-on time of approximately 26% of the R-R interval [138,167] (for single-source scanners, the minimum duration of active tube current is approximately one half of the rotation time plus the fan angle [194]). This method takes advantage of the large volume coverage available with 64-detector row CT (64 x 0.625 mm= 40 mm/4cm thick slabs of z-axis coverage) [122,167]. Patient's should have a low stable heart rate less than 65-70 beats per minute, low heart rate variability, and no arrhythmia [122,137,234,300]. For this exam, scanning is initiated at a predefined time after detcetion of an R-peak- typically during mid-to-late diastole -for example at 60% or 70% of the R-R interval [101,201,266]. Therefore, the x-ray beam is turned on for only a short portion of diastole when the data acquisition is considered relevant, and it is turned off during the remainder of the R-R cycle [138,145]. The projection data are acquired for only part of the complete gantry rotation (i.e.: a partial scan) [101]. Additional "padding" of the "tube-on" time is commonly employed (typically about 100 msec) [122,138]. This technique (padding) turns the tube on prior to, and leaves it on after, the pre-set acquisition time- this permits the reconstruction to adapt to minor heart rate variations in order to produce high quality images [122]. In other words, padding has potential for rendering a diagnosis in cases in which image interpretation in the selected phase is suboptimal, because multiple other phases are available for analysis [194]. The use of padding increases patient radiation exposure and for patients with excellent heart rate control, padding may not be necessary [194].
Following completion of the first acquisition, the table is then
moved to the next location for further data acquisition (i.e.:
this is a non-helical acquisition) [101]. The cycle is repeated
until the entire scan length is covered- typically 12-15 cm [101].
The result is very little overlap (5 mm) between the scans [122]
and the pitch is approximately 1 [300]. The average total scan
time is about 5 seconds with a total x-ray on time of about 1
second [122]. For wide array scanners (320 detector rows with 16
cm z-axis coverage), the entire heart may be covered in a single
gantry rotation [266]. The advantage of prospective triggering is
reduced radiation exposure because the projection data is not
acquired throughout the cardiac cycle [101,118]. With this
technique- mean effective doses have been reported to be 2.6-4.4
mSv (approximately 68-80% dose reduction compared to retrospective
gating), but doses about or below 1 mSv can be obtained in thin
patients [122,137,138,145,201]. Diagnostic performance has been
shown to be similar between prospective and retrospective CT
angiography exams [137,138]. Drawbacks of this technique are that
patients with high (above 65 bpm) are precluded due to the narrow
predefined reconstruction interval (higher heart rates produce
more motion artifacts) [145,295]. Also- the technique does not
work well if there is irregular heart rate due to reconstruction
stair-step artifacts [145,295]. Other disadvantages of prospective
gating include the inability to evaluate the cardiac valves, wall
motion, and other functional parameters as images can only be
reconstructed from the predefined phase of data acquisition
[145,266]. However, these limitations can be overcome with PET/CT
scanning in which myocardial perfusion and ventricular function
can be evaluated on the gated perfusion PET exam [149].
|
Prospective imaging: For prospective imaging- the x-ray beam is turned on for only a short period of time- this helps to minimize patient radiation exposure |
|
|
A dual-source scanner can acquire a prospective ECG-triggered
exam using high-pitch helical scanning if the patient's heart rate
is low (under 60 beats/min) and the patient has a low BMI (under
30) [266].
A retrospectively ECG gated
acquisition had been the preferred method for contrast enhanced
imaging of the coronary arteries [35]. Retrospective ECG gating
coronary CT requires a highly overlapping continuous spiral scan
(typical pitch is 0.2 to 0.4) with a table speed adapted to the
patients heart rate and simultaneous recording of the ECG trace
which is used for linkage of scan data with particular phases of
the cardiac cycle [35,101]. In other words, data is acquired
throughout the cardiac cycle with a continuous helical acquisition
and then retrospectively, projection data from selected points
within the R-R interval are selected for image reconstruction
[101]. Advantages of retrospective gating compared to prospective
gating include improved temporal resolution with
multisector/multicycle reconstruction, the ability to acquire
systolic phase information and ejection fraction, the ability to
assess ventricular and aortic valve motion, and the potential for
ECG editing [137]. Retrospectively gated techniques are also less
sensitive to arrhythmia [266]. The disadvantage of this type of
acquisition is increased patient radiation exposure [266].
Retrospectively gated studies can be reconstructed with partial
scan data or with segmental reconstruction [101]. For partial scan
reconstruction, the scan data required for reconstruction are
obtained by rotating the x-ray tube 180 degrees plus the fan angle
(30-60 degrees) of the CT detector assembly [101]. Therefore, the
temporal resolution will be slightly greater than one-half of the
gantry rotation time [101]. In multiple segmental reconstruction, the scan projection data to
perform a partial scan reconstruction are selected from various
sequential heart cycles, instead of from a single heart cycle
[101]. In other words- data from different parts of the heart
cycle are chosen, so that the sum of these segments equates to the
partial scan data required for image reconstruction [101]. This
results in improvement in temporal resolution [101]. The
disadvantage is that because projection data sets are obtained
from different heart beats, a mis-registration due to rapid motion
can result in degradation of image spatial resolution [101].
High-definition CT offers 2.5 times more views per rotation
compared to standard CT and substantially improves the in-plane
resolution to 0.23 mm and improves contrast resolution to 3 mm
[300].
Because image quality on CT is dominated by quantum noise
(mottle), the radiation dose is closely linked to diagnostic
accuracy and confidence [159]. Too low a radiation dose leads to
high-noise-level images that are nondiagnostic [159]. A drawback
of retrospective ECG gated CT is that it is associated with a
higher radiation dose to the patient [35] because of overlapping
data acquisition and acquiring data during cardiac phases that do
not contribute to image reconstruction [118]. With a
multi-detector row CT the radiation dose is approximately 7 to 21
mSv (0.7 to 2.1 rem) and is higher in women (1 mSv= 0.1 rem) [35,50,52,122]. The female breast can receive
an effective dose that is approximately 10 times that of a routine
mammogram [126]. Doses from dual-source CT systems are also
relatively high- ranging from 8-16 mSv [122]. The dose from
coronary CT imaging is higher than the dose from conventional
angiography (which is about 2.5-5.6 mSv) [50,51,78,122,141].
A JAMA review, found wide variability in the radiation dose
associated with 64-slice CT with an estimated dose of 12 mSv
(equivalent to the dose from 600 CXR's) [154]. The article
concluded that effective ways to reduce radiation exposure are
available and should be utilized when performing coronary CTA
[154]. Breast shielding using bismuth shields can reduce breast
radiation dose from 46-57%- however, at least one article using
breast phantoms has suggested that this shielding can result in
increased image noise and decrease tissue contrast that may affect
evaluation of the coronary arteries (i.e.- detection and
characterization of plaque) [255]. The use of breast shields for
coronary CTA are not presently recommended by the Society of
Cardiovascular Computed Tomography [259].
The radiation from CT imaging "may" pose a risk for increased
incidence of breast and lung cancer [111]. It has been calculated
that a 10 mSv dose may be associated with a 1 in 1000 to a 1 in
2000 lifetime cancer risk [122]. Therefore, a 15 mSv CT scan has a
range of risk for inducing a fatal cancer between
1 in 677 to 1 in 1333 [122] (to as high as 1 in 1900
[129]). One point to remember is that the excess lifetime risk of
radiation induced cancer mortality declines significantly with age
and that the majority of patients being evaluated for coronary
artery disease are often elderly [98,111]. Additionally, the
estimates are controversial and probably overestimated because of
recognized assumptions within the linear no threshold model used
for risk determination [259]. The excess relative risk for lung
and breast cancer after a single multidetector CT of the chest is
generally below 1% for individuals aged 55 years or older [111].
However, the lifetime excess risk for breast or lung cancer in
girls and young women aged 15-25 years that undergo a single
ECG-gated CT angiographic exam is higher- ranging from 1.7% to
5.5% for a single examination [111]. The estimated attributable
lifetime cancer risk after an ECG-gated coronary CT angiography
exam has been reported to be as high as 1 in 219 for a 20-year old
woman [160]. The risk for radiation induced cancer would be
increased in an additive manner if multiple follow-up exams were
performed [111]. One point to remember is that estimation of
radiation risks is based upon atomic bomb data [129]. There is a
certain amount of uncertainty when trying to account for
biological effectiveness between gamma rays and fast neutrons to
which atomic bomb survivors were exposed and x-rays from CTCA
exams [129].
To put the radiation dose into perspective, the dose for a
rest-stress myocardial perfusion exam using Tc99m is 8-17.5 mSv;
using thallium stress and reinjection its 18-25.1 mSv; and using a
dual isotope exam the dose is about 27.3 mSv (this is one reason
why dual isotope imaging has fallen out of favor) [122,190]. The
radiation dose is also comparable to the annual dose received from
naturally occurring sources of radiation such as radon and cosmic
radiation (1-10 mSv) [172]. For most CT examinations, the
potential risk of dying is less than that of drowning or of a
pedestrian dying from being struck by any form of ground
transportation [172]. The estimated life-time risk of death from
various sources have been described and can be reviewed for
comparison to radiation exposure (Epicardial adipose
tissue:
Epicardial adipose tissue located within the pericardial sac is
associated with impaired LV systolic function, atrial
fibrillation, cardiomyopathy, and particularly, coronary artery
disease [303]. Metabolic processes in the epicardial fat are
thought to affect atherosclerosis by endocrine and paracrine
mechanisms of secreted proinflammatory cytokines and adipokines
[303]. CT can be used to quantify the volume of epicardial adipose
tissue [303]. Greater volumes of epicardial adipose tissue have
been shown to be associated with a greater likelihood for
myocardial ischemia [303].
REFERENCES:
(1) Radiology 1980; 137(3): 609-616
(3) J Comput Assist Tomogr 1997; 21(4) 619-622
(4) Radiologic Clinics of North America 1999; Stanford W, Thompson BH. Imging of coronary artery calcification. Its importance in assessing atherosclerotic disease. 37(2): 257-272
(5) AJR 2000; Yoon HC, et al. Interscan variation in coronary artery calcium quantification in a large asymptomatic patient population. 174: 803-809
(6) AJR 2000; Becker CR, et al. Imaging of noncalcified coronary plaques using helical CT with retrospective ECG gating. 175: 423-24 (No abstract available)
(7) Radiology 2000; Ohnesorge B, et al. Cardiac imaging by means of electrocardiographically gated multisection spiral CT: Initial experience. 217: 567-571
(8) AJR 2000; Callister T, et al. Sensitivity of two electron beam tomography protocols for the detection and quantification of coronary artery calcium. 175: 1743-1746
(9) J Am Coll Cardiol 1990; Agatston AS, et al. Quantification of coronary artery calcium using ultrafast computed tomography. 15: 827-32
(10) Am J Cardiol 2000; O'Malley PG, et al. Prognostic value of coronary electron-beam computed tomography for coronary heart disease events in asymptomatic populations. 85: 945-948
(11) J Am Coll Cardiol 2001; Georhiou D, et al. Screening patients with chest pain in the emergency department using electron beam tomography: A follow-up study. 38: 105-110
(12) Radiology 2001; Mao S, et al. Effect of electrocardiogram triggering on reproducibility of coronary artery calcium scoring. 220: 707-711
(13) Radiology 2001; Hong C, et al. ECG-gated reconstructed multi-detector row CT coronary angiography: Effect of varying trigger delay on image quality. 220: 712-717
(14) Radiology 2001; Goldin JG, et al. Spiral versus electron-beam CT for coronary artery calcium scoring. 221: 213-221
(15) Radiology 2001; Kopp AF, et al. Coronary arteries: retrospectively ECG-gated multi-detector row CT angiograpgy with selective optimization of the image reconstruction window. 221: 683-688
(16) AJR 2001; Horiguchi J, et al. Quantification of coronary artery calcium using multidetector CT and a retrospective ECG-gating reconstruction algorithm. 177: 1429-1435
(17) Circulation 2000; He ZX, et al. Severity of coronary artery calcium by electron beam computed tomography predicts silent myocardial ischemia. 101: 244
(18) Radiology 2002; Kopp AF, et al. Reproducibility and accuracy of coronary calcium measurements with multi-detector row versus electron beam CT. 225: 113-119
(19) Radiology 2002; Hong C, et al. Coronary artery calcium measurement with multi-detector row CT: in vitro assessment of effect of radiation dose. 225: 901-906
(20) Radiology 2003; Hunold P, et al. Radiation exposure during cardiac CT: effective doses at multi-detector row CT and electron beam CT. 226: 145-152
(21) Radiology 2003; Hong C, et al. Coronary artery calcium quantification at multi-detector row CT: influence of heart rate and measurement methods on interacquisition variability- initial experience. 228: 95-100
(22) Radiology 2003; Takahashi N, Bae KT. Quanitification of coronary artery calcium with multi-detector row CT: assessing interscan variability with different tube currents- pilot study. 228: 101-106
(23) AJR 2003; Mahnken AH, et al. Detection of coronary calcifications: feasibility of dose reduction with a body weight-adapted examination protocol. 181: 533-538
(24) AJR 2003; Rumberger JA, Kaufman L. A rosetta stone for coronary calcium risk stratification: agatston, volume, and mass scores in 11,490 individuals. 181: 743-748
(25) Radiology 2003; Shaw LJ, et al. Prognostic value of cardiac risk factors and coronary artery calcium screening for all-cause mortality. 228: 826-833
(26) AJR 2003; Van Hoe LR, et al. Coronary artery calcium scoring using ECG-gated multidetector CT: effect of individually optimized image-reconstruction window on image quality and measurement reproducibility. 181: 1093-1100
(27) Radiology 2003; Viegenthart R, et al. Coronary calcifcation at electron-beam CT: effect of section thickeness on calcium scoring in vitro and in vivo. 229: 520-525
(28) JAMA 2004; Greenland P, et al. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. 291: 210-215
(29) J Nucl Cardiol 2003; Moser KV, et al. Coronary calcium screening in asymptomatic patients as a guide to risk factor modication and stress myocardial perfusion imaging. 10: 590-598
(30) J Nucl Cardiol 2003; Cerqueira MD, Rumsey MP. Coronary calcium scoring: what does it really mean? 10: 692-695
(31) Radiology 2004; Stanford W, et al. Coronary artery calcium quantification at multi-detector row helical CT versus electron-beam CT. 230: 397-402
(32) AJR 2004; Hoffman MHK, et al. Noninvasive coronary imaging with MDCT in comparison to invasive conventional coronary angiography: a fast-developing technology. 182: 601-608
(33) AJR 2004; Desjardins B, Kazerooni EA. ECG-gated cardiac CT. 182: 993-1010
(34) Radiology 2004; Schoenhagen P, et al. Noninvasive imaging of the coronary arteries: current and future role of multi-detector row CT. 232: 7-17
(35) Radiology 2004; Schoepf UJ, et al. CT of coronary artery disease. 232: 18-37
(36) J Nucl Cardiol 2004; Anand DV, et al. Prevalence of silent myocardial ischemia in asymptomatic individuals with subclinical atherosclerosis detected by electron beam tomography. 11: 450-457
(37) Radiology 2004; Schlosser T, et al. Coronary artery calcium score: influence of reconstruction interval at 16-detector row CT with retrospective electrocardiographic gating. 233: 586-589
(38) Radiology 2004; Cademartiri F, et al. Intravenous contrast material administration at 16-detector row helical CT coronary angiography: test bolus versus bolus-tracking technique. 233: 817-823
(39) Radiology 2004; Hofmann LK, et al. Electrocardiographically gated 16-slice CT of the thorax: cardiac motion suppression. 233: 927-933
(40) Radiology 2004; Hoffmann MH, et al. Noninvasive coronary angiography with 16-detector row CT: effect of heart rate. 234: 86-97
(41) Radiology 2005; Yamamuro M, et al. Cardiac functional analysis with multi-detector row CT and segmental reconstruction algorithm: comparison with echocardiography, SPECT, and MR imaging. 234: 381-390
(42) AJR 2005; Halliburton SS, et al. Potential clinical impact of variability in the measurement of coronary artery calcium with sequential MDCT. 184: 643-648
(43) AJR 2005; Shim SS, et al. Improvement of image quality with beta-blocker premedication on ECG-gated 16-MDCT coronary angiography. 184: 649-654
(44) AJR 2005; Schlosser T, et al. Assessment of left ventricular parameters using 16-MDCT and new software for endocardial and epicardial border delineation. 184: 765-773
(45) J Nucl Cardiol 2005; Raggi P, Berman DS. Computed tomography coronary calcium screening and myocardial perfusion imaging. 12: 96-103
(46) J Nucl Cardiol 2005; Shaw LJ, et al. Computed tomography imaging within nuclear cardiology. 12: 131-142
(47) J Nucl Cardiol 2005; Miller DD, Shaw LJ. Screening for coronary heart disease: cardiology through the oncology looking glass. 12: 158-165
(48) Radiology 2005; Nelson JC, et al. Measuring coronary calcium on CT images adjusted for attenuation differences. 235: 403-414
(49) Radiology 2005; Lau GT, et al. Coronary artery stenoses: detection with calcium scoring, CT angiography, and both methods combined. 235: 415-422
(50) AJR 2005; Lawler LP, et al. MDC evaluation of the coronary arteries, 2004: how do we do it- data acquisition, postprocessing, display, and interpretation. 184: 1402-1412
(51) AJR 2005; Heuschmid M, et al. ECG-gated 16-MDCT of the coronary arteries: assessment of image quality and accuracy in detecting stenoses. 184: 1413-1419
(52) JAMA 2005; Hoffman MHK, et al. Noninvasive coronary angiography with multislice computed tomography. 293: 2471-2478
(53) AJR 2005; Horiguchi J, et al. Variability of repeated coronary artery calcium measurements by 16-MDCT with retrospective reconstruction. 184: 1917-1923
(54) Radiology 2005; Datta J, et al. Anomalous coronary arteries in adults: depiction at multi-detector row CT angiography. 235: 812-818
(55) J Nucl Med 2005; Hacker M, et al. Comparison of spiral mutlidetector CT angiography and myocardial perfusion imaging in the noninvasive detection of functionally relevant coronary artery lesions: first clinical experience. 46: 1294-1300
(56) J Nucl Cardiol 2005; Shaw LJ, Berman DS. Redefining the low-risk patient with signifncat atherosclerotic disease. 12: 375-377
(57) J Nucl Cardiol 2005; Thompson RC, et al. Clinical utility of coronary artery calcium scoring after nonischemic myocardial perfusion imaging. 12: 392-400
(58) Radiology 2005; Detrano RC, et al. Coronary calcium measurement: effect of CT scanner type and calcium measure on rescan reproducibility- MESA study. 236: 477-484
(59) Radiology 2005; Cademartiri F, et al. Intravenous contrast material administration at helical 16-detector row CT coronary angiography: effect of iodine concentration on vascular attenuation. 236: 661-665
(60) Radiology 2005; Shemesh J, et al. Coronary artery calcium measurement with multi-detector row CT and low radiation dose: comparison between 55 and 165 mAs. 236: 810-814
(61) Radiology 2006; Herzog C, et al. Multi-detector row CT coronary angiography: influence of reconstruction technique and heart rate on image quality. 238: 75-86
(62) AJR 2005; Dubinsky TJ. Coronary artery calcification scoring. 185: 1540-1541
(63) AJR 2005; Servukov AB, et al. Serial electron beam CT measurements of coronary artery calcium: has your patient's calcium score actually changed? 185: 1546-1553
(64) Radiology 2006; Herzog C, et al. Multi-detector row CT coronary angiography: influence of reconstruction technique and heart rate on image quality. 238: 75-86
(65) AJR 2006; Ghersin E, et al. 16-MDCT coronary angiography versus invasive coronary angiography in acute chest pain syndrome: a blinded prospective study. 186: 177-184
(66) AJR 2006; Sandstede JJW, et al. Different reconstruction intervals for exclusion of coronary artery calcifications by retrospectively gated MDCT. 186: 193-197
(67) AJR 2006; Cademartiri F, et al. Improving diagnostic accuracy of MDCT coronary angiography in patients with mild heart rhythm irregularities using ECG editing. 186: 634-638
(68) J Nucl Cardiol 2006; Scholte AJH, et al. Screening of asymptomatic patients with type 2 diabetes mellitus for silent coronary artery disease: combined use of stress myocardial perfusion imaging and coronary calcium scoring. 13: 11-18
(69) J Nucl Cardiol 2006; Di Carli MF, et al. Integrated cardiac PET-CT for the diagnosis and management of CAD. 13: 139-144
(70) J Nucl Cardiol 2006; Okwuosa T, et al. Coronary artery disease and nuclear imaging in renal failure. 13: 150-155
(71) J Nucl Med 2006; Hoffmann U, et al. Coronary CT angiography. 47: 797-806
(72) AJR 2006; Pannu HK, et al. β-blockers for cardiac CT: a primer for the radiologist. 186: S341-345
(73) AJR 2006; Abada HT, et al. MDC of the coronary arteries: feasibility of low-dose CT with ECG-pulsed tube current modulation to reduce radiation dose. 186: S387-390
(74) J Nucl Cardiol 2006; Rosman J, et al. Lack of correlation between coronary artery calcium and myocardial perfusion imaging. 13: 333-337
(75) AJR 2006; Nikolaou K, et al. Accuracy of 64-MDCT in the diagnosis of ischemic heart disease. 187: 111-117
(76) AJR 2006; Pannu HK, et al. Coronary CT angiography with MDCT: assessment of vessel visibility. 187: 119-126
(77) J Nucl Med 2006; Berman DS, et al. Roles of nuclear cardiology, cardiac computed tomography, and cardiac magnetic resonance: noninvasive risk stratification and a conceptual framework for the selection of noninvasive imaging tests in patients with known or suspected coronary artery disease. 47: 1107-1118
(78) Radiographics 2006; Hoffman U, et al. Cardiac CT in emergency department patients with acute chest pain. 26: 963-980
(79) J Nucl Cardiol 2006; Thomas GS. Coronary computed tomographic angiography: competitive or complementary? 13: 605-608
(80) J Nucl Cardiol 2006; Wackers FJT. Asymptomatic patients with diabetes mellitus should be screened for coronary artery disease. 13: 609-615
(81) AJR 2006; Hoffmann U, et al. MDCT in early triage of patients with acute chest pain. 187: 1240-1247
(82) Radiology 2006; Leschka S, et al. Noninvasive coronary angiography with 64-section CT: effect of average heart rate and heart rate variability on image quality. 241: 378-385
(83) J Nucl Med 2006; Schuijf JD, et al. A comparative regional analysis of coronary atherosclerosis and calcium score on multislice CT versus myocardial perfusion on SPECT. 47: 1749-1755
(84) J Nucl Cardiol 2006; Wyrick JJ, Wei K. Cardiac imaging in the evaluation of patients presenting to the emergency department with chest pain. 13: 749-755
(85) AJR 2007; Muhlenbruch G, et al. Evaluation of aortocoronary bypass stents with cardiac MDCT compared with conventional catheter angiography. 188: 361-369
(86) J Nucl Cardiol 2007; Pundziute G, et al. Impact of coronary calcium score on diagnostic accuracy of multislice computed tomography coronary angiography for detection of coronary artery disease. 14: 36-43
(87) Radiology 2007; Oncel D, et al. Coronary stent patency and in-stent restenosis: determination with 64-section multidetector CT coronary angiography- initial experience. 242: 403-409
(88) AJR 2007; Schlosser T, et al. Coronary artery calcium scoring: influence of reconstruction interval and reconstruction increment using 64-MDCT. 188: 1063-1068
(89) J Nucl Cardiol 2007; Cury RC, et al. Comprehensive cardiac CT study: evaluation of coronary arteries, left ventricular function, and myocardial perfusion- is it possible? 14: 229-243
(90) J Nucl Med 2007; Gaemperli O, et al. Cardiac image fusion from stand-alone SPECT and CT: Clinical experience. 48: 696-703
(91) J Nucl Med 2007; Di Carli MF, et al. Clinical myocardial perfusion PET/CT. 48: 783-793
(92) Radiology 2007; Schoepf UJ, et al. Coronary CT angiography. 244: 48-63
(93) Radiology 2007; Herzog C, et al. Significant coronary artery stenosis: comparison on per-patient and per-vessel or per-segment basis at 64-section CT angiography. 244: 112-120
(94) J Nucl Cardiol 2007; Beller GA. CT angiography: too much too soon. 14: 267-268
(95) J Nucl Cardiol 2007; Ho J, et al. Severe coronary artery calcifications are associated with ischemia in patients undergoing medical therapy. 14: 341-346
(96) Radiology 2007; Vanhoenacker PK, et al. Diagnostic performance of multidetector CT angiography for assessment of coronary artery disease: meta-analysis. 244: 419-428
(97) AJR 2007; Matt D, et al. Dual-source CT coronary angiography: image quality, mean heart rate, and heart rate variability. 189: 567-573
(98) AJR 2007; Feuchter GM, et al. Diagnostic performance of 64-slice computed tomography in evaluation of coronary artery bypass grafts. 189: 574-580
(99) AJR 2007; Kroft LJM, et al. Artifacts in ECG-synchronized MDCT coronary angiography. 581-591
(100) J Nucl Med 2007; Schepis T, et al. Added value of coronary artery calcium score as an adjunct to gated SPECT for the evaluation of coronary artery disease in an intermediate-risk population. 48: 1424-1430
(101) Radiographics 2007; Mahesh M, Cody DD. Physics of cardiac imaging with multiple-row detector CT. 27: 1495-1509
(102) Radiographics 2007; O'Brien JP, et al Anatomy of the heart at multidetector CT: what the radiologist needs to know. 27: 1569-1582
(102) J Nucl Cardiol 2007; Schuijf JD, et al. The current status of multislice computed tomography in the diagnosis and prognosis of coronary artery disease. 14: 604-612
(103) Radiology 2007; Schuijf JD, et al. Evaluation of patients with previous coronary stent implantation with 64-section CT. 245: 416-423
(104) Radiology 2007; Das KM, et al. Contrast-enhanced 64-section coronary mutlidetector CT angiography versus conventional coronary angiography for stent assessment. 245: 424-432
(105) AJR 2007; Leontiev O, Dubinsky TJ. CT-based calcium scoring to screen for coronary artery disease: why aren't we there yet? 189: 1061-1063
(106) J Nucl Cardiol 2007; Rozanski A, et al. Use of coronary calcium scanning for predicting inducible myocardial ischemia: influence of patients clinical presentation. 14: 669-79
(107) Radiographics 2006; Pugliese F, et al. Multidetector CT for visualization of coronary stents. 26: 887-904
(108) Radiographics 2007; O'Brien JPO, et al. Anatomy of the heart at multidetector CT: what the radiologist needs to know. 27: 1569-1582
(109) Radiology 2007; Oncel D, et al. Effectiveness of dual-source CT coronary angiography for evaluation of coronary artery disease in patients with atrial fibrillation: initial experience. 245: 703-711
(110) Radiology 2007; Harmon M, et al. Coronary arteries: diagnostic performance of 16- versus 64-section spiral CT compared with invasive coronary angiography- meta-analysis. 245: 720-731
(111) Radiology 2007; Hurwitz LM, et al. Radiation dose from contemporary cardiothoracic multidetector CT protocols with an anthropomorphic female phantom: implications for cancer induction. 245: 742-750
(112) J Nucl Cardiol 2007; Di Carli MF, et al. Relationship between CT coronary angiography and stress perfusion imaging in patients with suspected ischemic heart disease assessed by integrated PET-CT imaging. 14: 799-809
(113) AJR 2007; Seifarth H, et al. Optimal systolic and diastolic reconstruction windows for coronary CT angiography using dual-source CT. 189: 1317-1323
(114) AJR 2007; Liu X, et al. Comparison of 3D free-breathing coronary MR angiography and 64-MDCT angiography for detection of coronary stenosis in patients with high calcium scores. 189: 1326-1332
(115) AJR 2007; Duerinckx AJ. Can the targeted use of MR angiography after CT angiography help assess the severity of focal calcific coronary lesions? 189: 1333-1334
(116) AJR 2008; Decramer I, et al. Effects of sublingula nitroglycerin on coronary lumen diameter and number of visualized septal branches on 64-MDCT angiography. 190: 219-225
(117) Radiology 2008; Kim DJ, et al. Saline flush effect for enhancement of aorta and coronary arteries at multidetector CT coromary angiography. 246: 110-115
(118) AJR 2008; Horiguchi J, et al. Radiation dose, image quality, stenosis measurement, and CT densitometry using ECG-triggered coronary 64-MDCT angiography" a phantom study. 190: 315-320
(119) J Nucl Cardiol 2008; Yerramasu A, et al. Cardiac computed tomography and myocardial perfusion imaging for risk stratification in asymptomatic diabetic patients: a critical review. 15: 13-22
(120) J Nucl Cardiol 2008; Di Carli MF, Hachamovitch R. Hybrid PET/CT is greater than the sum of its parts. 15: 118-122
(121) AJR 2008; Bae KT, et al. Contrast enhancement in cardiovascular MDCT: effect of body weight, height, body surface area, body mass index, and obesity. 190: 777-784
(122) Radiology 2008; Earls JP, et al. Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. 246: 742-753
(123) J Nucl Med 2008; Vesely MR, Dilsizian V. Nuclear cardiac stress testing in the era of molecular medicine. 49: 399-413
(124) J Nucl Med 2008; Sato A, et al. Quantitative measures of coronary stenosis severity by 64-slice CT angiography and relation to physiologic significance of perfusion in nonobese patients: comparison with myocardial perfusion imaging. 49: 564-572
(125) Radiology 2008; Brodoefel H, et al. Dual-source CT: effect of heart rate, heart rate variability, and calcification on image quality and diagnostic accuracy. 247: 346-355
(126) J Nucl Cardiol 2008; Castronovo FP. Regarding the patient dosimetry and cancer risk associated with performing computed tomography coronary angiography. 15: 157-158
(127) J Nucl Cardiol 2008; Vashist A, Bonow RO. Screening for coronary atherosclerosis with coronary calcium scoring: the "shape" of things to come? 15: 162-169
(128) J Nucl Cardiol 2008; Dhakshinamurthy VA, et al. Evaluation of graft patency by computed tomographic angiography in symptom-free post-coronary artery bypass surgery patients. 15: 201-208
(129) J Nucl Cardiol 2008; Einstein AJ, et al. Radiation dose and cancer risk estimates in 16-slice computed tomography coronary angiography. 15: 232-240
(130) Radiology 2008; Brown ER, et al. Coronary calcium coverage score: determination, correlates, and predictive accuracy in the multiethnic study of atherosclerosis. 247: 669-678
(131) Radiology 2008; Hamon M, et al. Diagnostic performance of 16- and 64-section spiral CT for coronary artery bypass graft assessment: meta-analysis. 247: 679-686
(132) AJR 2008; Leschka S, et al. Effect of decrease in heart rate variability on the diagnostic accuracy of 64-MDCT coronary angiography. 190: 1583-1590
(133) AJR 2008; Rademaker J, et al. Coronary artery disease after radiation therapy for Hodgkin's lymphoma: coronary CT angiography findings and calcium scores in nine asymptomatic patients. 191: 32-37
(134) AJR 2008; Kelly JL, et al. Coronary CT angiography findings in patients without coronary calcification. 191: 50-55
(135) AJR 2008; Oncel D, et al. Evaluation of coronary stent patency and in-stent restenosis with dual-source CT coronary angiography without heart rate control. 191: 56-63
(136) Radiology 2008; Gaemperli O, et al. Functionally relavant coronary artery disease: comparison of 64-section CT angiography with myocardial perfusion SPECT. 248: 414-423
(137) Radiology 2008; Hirai N, et al. Prospective versus retrospective ECG-gated 64-detector coronary CT angiography: assessment of image quality, stenosis, and radiation dose. 248: 424-430
(138) Radiology 2008; Shuman WP, et al. Prospective versus retrospective ECG gating for 64-detector CT of the coronary arteries: comparison of the image quality and patient radiation dose. 248: 431-437
(139) J Nucl Cardiol 2008; Nicol ED, et al. Comparison of 64-slice cardiac computed tomography with myocardial perfusion scintigraphy for assessment of global and regional myocardial function and infarction in patients with low to intermediate likelihood of coronary artery disease. 15: 497-502
(140) J Nucl Cardiol 2008; Scholte AJ, et al. Different manifestations of coronary artery disease by stress SPECT myocardial perfusion imaging, coronary calcium scoring, and multislice CT coronary angiography in asymptomatic patients with type 2 diabetes mellitus. 15: 503-509
(141) J Nucl Cardiol 2008; Cury RC, et al. Acute chest pain imaging in the emergency department with cardiac computed tomography angiography. 15: 564-575
(142) Radiology 2008; Weustink AC, et al. Optimal electrocardiographic pulsing windows and heart rate: effect on image quality and radiation exposure at dual-source coronary CT angiography. 248: 792-798
(143) J Nucl Cardiol 2008; Nicol ED, et al. Sixty-four-slice computed tomography coronary angiography compared with myocardial perfusion scintigraphy for the diagnosis of functionally significant coronary stenoses in patients with a low to intermediate likelihood of coronary artery disease. 15: 311-318
(144) Radiology 2008; Min JK, et al. Costs and clinical outcomes after coronary multidetector CT amgiography in patients without known coronary artery disease: comparison to myocardial perfusion SPECT. 249: 62-70
(145) Radiology 2008; Stolzmann P, et al. Dual-source CT in step-and-shoot mode: noninvasive coronary angiography with low radiation dose. 249: 71-80
(146) Radiology 2008; Lim HB, et al. Coronary stent fracture: detection with 64-section multidetector CT angiography in patients and in vitro. 249: 810-819
(147) AJR 2008; Matsumoto H, et al. ECG-edited middiastolic phase reconstruction improves image quality at 64-MDCT coronary angiography of patients with atrial fibrillation. 191: 1659-1666
(148) AJR 2008; Joemai RMS, et al. Automated cardiac phase selection with 64-MDCT coronary angiography. 191: 1690-1697
(149) J Nucl Cardiol 2008; Javadi M, et al. Lowering radiation dose for integrated assessment of coronary morphology and physiology: first experience with step-and-shoot CT angiography in a rubidium 82 PET-CT protocol. 15: 783-790
(150) J Nucl Cardiol 2008; Akram K, et al Coronary arterial atherosclerotic plaque imaging by contrast-enhanced computed tomography: fantasy or reality. 15: 818-829
(151) J Nucl Cardiol 2008; Akram K, et al. Coronary arterial atherosclerotic plaque imaging by contrast-enhanced computed tomography: fantasy or reality? 15: 818-829
(152) J Nucl Cardiol 2008; Nishimura M, Ono T. Clinical utility of myocardial fatty acid imaging in patients with end-stage renal disease. 15: 830-837
(153) AJR 2009; Johnson KM, et al. Traditional clinical risk assessment tools do not accurate predict coronary atherosclerotic plaque burden: a CT angiography study. 192: 235-243
(154) JAMA 2009; Hausleiter J, et al. Estimated radiation dose associated with cardiac CT angiography. 301: 500-507
(155) AJR 2009; Sundaram B, et al. Anatomy and terminology for the interpretation and reporting of cardiac MDCT: Part I, structured report, coronary calcium screening, and coronary artery anatomy. 192: 574-583
(156) AJR 2009; Sundaram B, et al. Anatomy and terminology for the interpretation and reporting of cardiac MDCT: Part 2, CT angiography, cardiac function assessment, and noncoronary and extracardiac findings. 192: 584-598
(157) AJR 2009; Budoff MJ, et al. Reproducibility of coronary artery calcified plaque with cardiac MDCT: the multi-ethnic study of atherosclerosis. 192: 613-617
(158) AJR 2009; Tatsugami F, et al. Evaluation of a body mass index-adapted protocol for low-dose 64-MDCT coronary angiography with prospective ECG triggering. 192: 635-638
(159) AJR 2009; Mayo JR, Leipsic JA. Radiation dose in cardiac CT. 192: 646-653
(160) AJR 2009; Pflederer T, et al. Image quality in a low radiation exposure protocol for retrospectively ECG-gated coronary CT angiography. 192: 1045-1050
(161) AJR 2009; Donnino R, et al. Dual-source versus single-source cardiac CT angiography: comparison of diagnostic image quality. 192: 1051-1056
(162) J Nucl Cardiol 2009; Griver-McKay M. Imaging diabetes mellitus with coronary computed tomography angiography, cardiovascular magnetic resonance, and positron emission tomography. 16: 135-138
(163) J Nucl Cardiol 2009; Wann S, et al. Cardiac computed tomographic angiography: evaluation of structures. 16: 139-150
(164) J Nucl Med 2009; Fox JJ, Strauss HW. Onestep closer to imaging vulnerable plaque in the coronary arteries. 50: 497-500
(165) J Nucl Cardiol 2009; Kaufmann PA, Gaemperli O. Combining CT and nuclear: a winning hybrid team. 16: 170-172
(166) J Nucl Cardiol 2009; Santana CA, et al. Diagnostic performance of fusion of myocardial perfusion imaging (MPI) and computed tomography coronary angiography. 16: 201-211
(167) AJR 2009; Shuman WP, et al. Whole-chest 64-MDCT of emergency department patients with nonspecific chest pain: radiation dose and coronary artery image quality with prospective ECG triggering versus retrospective ECG gating. 192: 1662-1667
(168) JAMA 2009; Raff GL, et al. Radiation dose from cardiac computed tomography before and after implementation of radiation dose-reduction techniques. 301: 2340-2348
(169) J Nucl Cardiol 2009; Nucifora G, et al. Prevalence of coronary artery disease across the Framingham risk categories: coronary artery calcium scoring and MSCT coronary angiography. 16: 368-375
(170) J Nucl Cardiol 2009; Sambuceti G, et al. Witnessing ischemia or proofing coronary atherosclerosis: two different windows on the same or on idfferent pathways precipitating cardiovascular events? 16: 447-455
(171) J Nucl Cardiol 2009; Cyrus T, et al Coronary CT angiography (CCTA) and advances in CT plaque imaging. 16: 466-473
(172) AJR 2009; McCollough CH, et al. In defense of body CT. 193: 28-39
(173) AJR 2009; May JM, et al. Low-risk patients with chest pain in the emergency department: negative 64-MDCT coronary angiography may reduce length of stay and hospital charges. 193: 150-154
(174) J Nucl Med 2009; Shaw LJ, Narula J. Risk assessment and predictive value of coronary artery disease testing. 50: 1296-1306
(175) AJR 2009; Bastarrika G, et al. Cardiac CT in the assessment of acute chest pain in the emergency department. 193: 397-409
(176) AJR 2009; Bauer RW, et al. Noncalcified atherosclerotic plaque burden at coronary CT angiography: a better predictor of ischemia at stress myocardial perfusion imaging than calcium score and stenosis severity. 193: 410-418
(177) J Nucl Cardiol 2009; Bart BA, et al. Comparison of dobutamine stress echocardiography, dobutamine SPECT, and adenosine SPECT myocardial perfusion imaging in patients with end-stage renal disease. 16: 507-515
(178) AJR 2009; Husmann L, et al. Low-dose coronary CT angiography with prospective ECG triggering: validation of a contrast material protocol adapted to body mass index. 193: 802-806
(179) Radiology 2009; Uebleis C, et al. Stable coronary artery disease: prognostic value of myocardial perfusion SPECT in relation to coronary calcium scoring - long-term followup. 252: 682-690
(180) Radiology 2009; Baumuller S, et al. Dual-source versus 64-section CT coronary angiography at lower heart rates: comparison of accuracy and radiation dose. 253: 56-64
(181) J Nucl Cardiol 2009; Abidov A, et al. Clinical effectiveness of coronary computed tomography angiography in the triage of patients to cardiac catheterization and revascularization after inconclusive stress testing: results of a 2-year prospective trial. 16: 701-713
(182) Radiology 2009; Bastarrika G, et al. CT of coronary artery disease. 253: 317-338
(183) J Nucl Cardiol 2009; Berman DS, et al. Screening for coronary artery disease in diabetic patients: a commentary. 16: 851-854
(184) J Nucl Cardiol 2009; Wackers FJT, Young LH. Lessons learned from the detection of ischemia in asymptomatic diabetics (DIAD) study. 16: 855-859
(185) J Nucl Cardiol 2009; Narula J. Who gets the heart attack: noninvasive imaging markers of plaque instability. 16: 860-868
(186) J Nucl Cardiol 2009; van Werkhoven JM, et al. The value of multi-slice-computed tomography coronary angiography for risk stratification. 16: 970-980
(187) J Nucl Cardiol 2009; Healy KO, et al. Prognosis and coronary computed tomographic angiography: current and emerging concepts. 16: 981-988
(188) AJR 2010; Wykrzykowska JJ, et al. Assessment of in-stent restenosis using 64-MDCT analysis of the CORE-64 multicenter international trial. 194: 85-92
(189) Radiology 2010; Min JK, et al. Cost-effectiveness of coronary CT angiography versus myocardial perfusion SPECT for evaluation of patients with chest pain and no known coronary artery disease. 254: 801-808
(190) J Nucl Cardiol 2010; Beller GA. Importance of consideration of radiation doses from cardiac imaging procedures and risks of cancer. 17: 1-3
(191) J Nucl Cardiol 2010; Gaemperli O, Kaufmann PA. Multimodality cardiac imaging. 17: 4-7
(191) J Nucl Cardiol 2010; Budoff MJ, Hacioglu Y. Coronary CT angiography offers further risk stratification in the management of patients with normal SPECT results. 17: 13-15
(192) J Nucl Cardiol 2010; Sato A, et al. Incremental value of combining 64-slice computed tomography angiography with stress nuclear myocardial perfusion imaging to improve noninvasive detection of coronary artery disease. 17: 19-26
(193) J Nucl Cardiol 2010; Choudhary G, et al. The role of calcium score and CT angiography in the medical management of patients with normal myocardial perfusion imaging. 17: 45-51
(194) AJR 2010; LeBounty TM, et al. Effect of padding duration on radiation dose and image interpretation in prospectively ECG-triggered coronary CT angiography. 194: 933-937
(195) JAMA 2010; Polonsky TS, et al. Coronary artery calcium score and risk classification for coronary heart disease prediction. 303: 1610-1616
(196) J Nucl Cardiol 2010; Blankstein R, Dorbala S. Adding calcium scoring to myocardial perfusion imagnig: does it alter physicians' therapeutic decision making? 17: 168-171
(197) J Nucl Cardiol 2010; Bybee KA, et al. Diagnostic and clinical benefit of combined coronary calcium and perfusion assessment in patients undergoing PET/CT myocardial perfusion stress imaging. 17: 188-196
(198) AJR 2010; Johnson KM, Dowe DA. The detection of any coronary calcium outperforms Framingham risk score as a first step in screening for coronary atherosclerosis. 194: 1235-1243
(199) AJR 2010; Halpern EJ, et al. Cost-effectiveness of coronary CT angiography in evaluation of patients without symptoms who have positive stress test results. 194: 1257-1262
(200) J Nucl Cardiol 2010; Carrabba N, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography for the detection of in-stent restenosis: a meta-analysis. 17: 470-480
(201) AJR 2010; Bischoff B, et al. Comparison of sequential and helical scanning for radiation dose and image quality: results of the prospective multicenter study on radiation dose estimates of cardiac CT angiography (PROTECTION) I study. 194: 1495-1499
(202) Radiology 2010; Van Werkhoven JM, et al. Diabetes: prognostic value of CT coronary angiography- comparison with a nondiabetic population. 256: 83-92
(203) AJR 2010; Leipsic J, et al. Adaptive stastical
reconstruction: assessment of image noise and image quality
in coronary CT angiography. 649-654
(204) AJR 2010; Leipsic J, et al. Estimated radiation dose reduction using adaptive statistical iterative reconstruction in coronary CT angiography: the ERASIR study. 655-660
(205) AJR 2010; Shuman WP, et al. Negative ECG-gated cardiac CT in patients with low-to-moderate risk chest pain in the emergency department: 1-year follow-up. 195: 923-927
(206) J Nucl Cardiol 2010; Beller GA. Chronic kidney disease and risk for coronary events: value of myocardial perfusion imaging. 17: 759-760
(207) J Nucl Cardiol 2010; Yerramasu A, et al. Comparative roles of cardiac CT and myocardial perfusion scintigraphy in the evaluation of patients with coronary artery disease: competitive or complementary. 17: 761-770
(208) J Nucl Cardiol 2010; Tamarappoo BK, et al. Assessment of the relationship between stenosis severity and distribution of coronary artery stenoses on multislice computed tomographic angiography and myocardial ischemia on single photon emission computed tomography. 17: 791-802
(209) Radiology 2010; Mahabadi AA, et al. Safety, efficacy, and indications of β-adrenergic receptor blockade to reduce heart rate prior to coronary CT amgiography. 257: 614-623
(210) AJR 2010; van der Bijl N, et al. Assessment of agatston coronary artery calcium score using contrast-enhanced CT coronary angiography. 195: 1299-1305
(211) AJR 2010; Sommer WH, et al. Feasibility and radiation dose of high-pitch acquisition protocols in patients undergoing dual-source cardiac CT. 195: 1306-1312
(212) J Nucl Cardiol 2011; de Graaf FR, et al. Incremental prognostic value of left ventricular function analysis over non-invasive coronary angiography with multidetector computed tomography. 17: 1034-1040
(213) J Nucl Cardiol 2011; Abidov A, Ragg GL. Value of coronary CTA in patients with known or suspected CAD and non-diagnostic initial myocardial perfusion testing: current evidence and clinical considerations. 17: 1101-1106
(214) AJR 2011; Dupont MVM, et al. Right ventricle function assessment by MDCT. 196: 77-86
(215) Radiographics 2011; Caudron J, et al. Evaluation of left ventricular diastolic function with cardiac MR imaging. 31: 239-261
(216) J Cardiovasc Comput Tomogr 2011; Raff GL. Radiation does from coronary CT angiography: five years if progress. 4: 365-374
(217) J Cardiovasc Comput Tomogr 2011; Qian Z, et al. Lesion- and vessel-specific coronary artery calcium scores are superior to whole-heart Agatston and volume scores in the diagnosis of obstructive coronary artery disease. 4: 391-399
(218) J Cardiovasc Comput Tomogr 2010; Farb A. From histology to computed tomography: every picture tells a story. 4: 309-311
(219) J Cardiovasc Comput Tomogr 2010; Pagali SR, et al. Interobserver variations of plaque severity score and segment stenosis score in coronary arteries using 64 slice multidetector computed tomography: a substudy of the ACCURACY trial. 4: 312-318
(220) J Cardiovasc Comput Tomogr 2011; Budoff MJ, Malpeso JM. Is coronary calcium the key to assessment of cardiovascular risk in asymptomatic adults? 5: 12-15
(221) J Cardiovasc Comput Tomogr 2011; Villines TC, et al. Calcium scoring and chest pain: is it dead on arrival? 5: 30-34
(222) J Nucl Cardiol 2011; Hendel RC. et al. The role of radionuclide myocardial perfusion imaging for asymptomatic individuals. 18: 3-15
(223) AJR 2011; Leipsic J, et al. A prospective randomized controlled trial to assess the diagnostic performance of reduced tube voltage for coronary CT angiography. 801-806
(224) J Cardiovasc Comput Tomogr 2011; Voros S, et al. Guideline for minimizing radiation exposure during acquisition of coronary artery calcium scans with the use of multidetector computed tomography. 5: 75-83
(225) J Cardiovasc Comput Tomogr 2011; Cheezum MK, et al. Cardiac CT angiography compared with myocardial perfusion stress testing on downstream resource utilization. 5: 101-109
(226) J Nucl Cardiol 2011; Rozanski A, et al. Comparison of the atherosclerotic burden among symptomatic patients vs matched volunteers. 18: 291-298
(227) J Nucl Cardiol 2011; Cury RC, et al. Cardiac CT in the
emergency department: convincing evidence, but cautious
implementation. 18: 331-341
(228) J Nucl Cardiol 2011; Beller GA. Noninvasive cardiovascular
imaging in primary prevention: does it influence management and
outcomes. 18: 383-384
(229) J Nucl Cardiol 2011; Peix A, et al. Interrelationship
between myocardial perfusion imaging, coronary artery calcium
score, and endothelial function in asymptomatic diabetics and
controls. 18: 398-406
(230) J Nucl Cardiol 2011; Hakeem A, et al. Non-invasive risk
assessment in patients with chronic kidney disease. 18: 472-485
(231) J Nucl Med 2011; Tamarappoo B, Hachamovitch R. Myocardial
perfusion imaging versus CT coronary angiography: when to use
which? 52: 1079-1086
(232) Radiology 2011; Nasis A, et al. Acute chest pain
investigation: utility of cardiac CT angiography in guiding
troponin measurement. 260: 381-389
(233) Radiology 2011; Renker M, et al. Evaluation of heavily
calcified vessels with coronary CT angiography: comparison of
iterative and filtered back projection image reconstruction. 260:
390-399
(234) J Cardiovasc Comput Tomogr 2011;
Halliburton S, et al. SCCT guidelines on radiation dose and
dose-optimization strategies in cardiovascular CT. 5: 198-224
(235) J Nucl Cardiol 2011; Beller GA. Imaging
of vulnerable plaques: will it affect patient management and
influence outcomes? 18: 531-533
(236) J Nucl Cardiol 2011; Hecht HS.
Controversies in nuclear cardiology: CT calcium scoring should
be rooutinely performed in patients undergoing myocardial
perfusion imaging who have a normal test result (and should be
routinely performed before myocardial perfusion imaging)-pro.
18: 695-696
(237) J Nucl Cardiol 2011; Hacker M, Becker
C. The incremental value of coronary artery calcium scores to
myocardial single photon emission computed tomography in risk
assessment. 18: 700-711
(238) Radiographics 2011; Stolzmann P, et al.
Complementary value of cardiac FDG PET and CT for the
characterization of atherosclerotic disease. 31: 1255-1269
(239) J Cardiovasc Comput Tomogr 2011; Nelson
RC, et al. New iterative reconstruction techniques for
cardiovascular computed tomography: how do they work, and what
are the advantages and disadvantages? 5: 286-292
(240) Radiology 2011; Vavere AL, et al.
Coronary artery stenoses: accuracy of 64-detector row CT
angiography in segments with mild, moderate, or severe
calcification- a subanalysis of the CORE-64 trial. 261: 100-108
(241) Radiology 2011; Neefkes LA, et al.
Image quality and radiation exposure using different low-dose
scan protocols in dual-source CT coronary angiography:
randomized study. 261: 779-786
(242) AJR
2012; Nakazono T, et al. HIV-related cardiac complications: CT and
MRI findings. 198: 364-369
(243) J Nucl Cardiol 2012; Beller GA. Nonobstructive coronary
atery disease on CT coronary angiography and abnormal coronary
flow reserve: two sides of the same coin. 19: 9-10
(244) J Nucl Cardiol 2012; Kral BG, et al. Severity of inducible
myocardial ischemia predicts incident acute coronary syndromes in
asymptomatic individuals with a family history of premature
coronary artery disease. 19: 28-36
(255) J Nucl Cardiol 2012; Einstein AJ, et al. Effect of bismuth
breast shielding on radiation dose and image quality in coronary
CT angiography. 19: 100-108
(256) AJR 2012; Ko SM, et al. Diagnostic performance of combined
noninvasive anatomic and functional assessment with dual-source CT
and adenosine-induced stress dual-energy CT for detection of
significant coronary stenosis. 198: 512-520
(257) AJR 2012; Wang Y, et al. Adenosine-stress dynamic
myocardialperfusion imaging with second-generation dual source CT:
comparison with conventional catheter coronary angiography and
SPECT nuclear myocardial perfusion imaging. 198: 521-529
(258) AJR 2012; Vliegenthart R, et al. CT of coronary heart
diseae: part I, CT of myocardial infarction, ischemia, and
viability. 198: 531-547
(259) J Cardiovasc Comput Tomogr 2012; Simprini LA, Taylor AJ.
Cardiac CT in women: clinical application and considerations. 6:
71-77
(260) J Cardiovasc Comput Tomogr 2012; Salavati A, et al.
Dual-source computed tomography angiography for diagnosis and
assessment of coronary artery disease: sysematic review and
meta-analysis. 6: 78-90
(261) J Cardiovasc Comput Tomogr 2012; Achenbach S, et al.
Influence of heart rate and phase of the cardiac cycle on the
occurence of motion artifact in dual-source CT angiography of the
coronary arteries. 6: 91-98
(262) J Cardiovasc Comput Tomogr 2012; Dey D, et al. Low
radiation coronary calcium scoring by dual-source CT with tube
current optimization based on patient body size. 6: 113-120
(263) J Nucl Cardiol 2012; Samad Z, et al. A meta-analysis and
systemic review of computed tomography angiography as a diagnostic
triage tool for patients with chest pain presenting to the
emergency department. 19: 364-376
(264) J Nucl Cardiol 2012; Alexanderson E, et al. Prognostic
value of cardiovascular CT: is coronary artery calcium screening
enough? The added value of CCTA. 19: 601-608
(265) J Nucl Med 2012; Ghadri JR, et al. Coronary calcium score
as an adjunct to nuclear myocardial perfusion imaging for risk
stratification before noncardiac surgery. 53: 1081-1086
(266) J Cardiovasc Comput Tomogr 2012; Halliburton S, et al.
Sate-of-the-art in CT hardware and scan modes for cardiovascular
CT. 6: 154-163
(267) J Cardiovasc Comput Tomogr 2012; Leipsic J, et al. Effect
if a novel vendor-specific motion correction algorithm on image
quality and diagnostic accuracy in persons undergoing coronary CT
angiography without rate-controled medications. 6: 164-171
(268) J Cardiovasc Comput Tomogr 2012; Lee AM, et al. Coronary
computed tomography angiography during arrhythmia: radiaiton dose
reduction with the prospectively ECG-triggered axial and
retrospectively ECG-gated helical 128-slice dual source CT. 6:
172-183
(269) J Nucl Cardiol 2012; Chinnalyan KM, et al. Coronary CT
angiography after stress testing: an efficient use of resources?
Implications of the advanced cardiovascular imaging consortium
(ACIC) results. 19: 649-57
(270) J Nucl Cardiol 2012; Otaki Y, et al. What have we learned
from CONFIRM? Prognostic implicaitons from a prospective
multicenter international observational cohort study of
consecutive patients undergoing coronary computed tomographic
angiography. 19: 787-795
(271) Radiology 2012; Nasir K, Clouse M. Role of nonenhanced
multidetector CT coronary artery calcium testing in asymptomatic
and symptomatic individuals. 264: 637-649
(272) Radiology 2012; Nance JW, et al. Incremental prognostic
value of different components of coronary atherosclerotic plaque
at cardiac CT angiography beyond coronary calcification in
patients with acute chest pain. 264: 679-690
(273) Radiology 2012; Moscariello A, et al. Coronary CT
angiography versus conventional cardiac angiography for
therapeutic decision making in patients with high likelihood of
coronary artery disease. 265: 385-392
(274) J Nucl Cardiol 2012; Joshi PH, et al. What is the role of calcium scoring in the age of coronary computed tomographic angiography. 19: 1226-1235
(275) AJR 2013; Cury RC, et al. Triage of patients presenting
with chest pain to the emergency department: implementation of
coronary angiography in a large urban health care system. 200:
57-65
(276) AJR 2013; Torres FS, et al. Coronary calcium scan
acquisition before coronary CT angiography: limited benefit or
useful addition? 200: 66-73
(277) Radiology 2013; Li M, et al Obstructive coronary artery
disease: reverse attenuation gradient sign at CT indicates distal
retrograde flow- a useful sign for differentiating chronic total
occlusion from subtotal occlusion. 266: 766-772
(278) Radiology 2013; Chen MY, et al. Submillisievert median
radiation dose for coronary angiography with a second-generation
320-detector row CT scanner in 107 consecutive patients. 267:
76-85
(279) J Cardiovasc Comput Tomogr 2013; Marwan M, et al. Very low-dose coronary arry sning with high-pitch spiral acquisition mo: comparison between 120-kV and 100-kV tube vtage p. 7: 32-38
(280) J Cardiovasc Comput Tomogr 2013; Deprez FC, et al.
Controversies about effects of low-kilovolatge MDCT acquisition on
Agatston calcium scoring. 7: 58-61
(281) Radiology 2013; Mouden M, et al. Coronary artery calcium
scoring to exclude flow-limiting coronary artery disease in
symptomatic stable patients at low or intermediate risk. 269:
77-83
(282) J Nucl Cardiol 2013; Petretta M, et al. Detection of silent
myocardial ischemia: is it clinically relevant? 20: 707-710
(283) J Nucl Cardiol 2013; Rozansji A, et al. The coronary
calcium tredmill test: a new approach to the initial workup of
patients with suspected coronary artery disease: 20: 719-730
(284) J Nucl Cardiol 2013; Hakeem A, et al. Does hybrid imaging
have a role in cardiac risk evaluaiton of the pre-renal transplant
patient? 20: 963-965
(285) J Cardiovasc Comput Tomogr 2013; Budoff MJ, et al. A
comparison of outcomes with coronary artery calcium scanning in
unselected populations: the Multi-ethnic study of atherosclerosis
(MESA) and Heinz Nixdorf RECALL study (HNR). 7: 182-191
(286) J Cardiovasc Comput Tomogr 2013; Yamamoto H, et al.
Noncalcified atherosclerotic lesions with vulnerable
characteristics detected by coronary CT angiography and future
cardiac events. 7: 192-199
(287) J Cardiovasc Comput Tomogr 2013; Daga N, et al. Prevalence
and severity of coronary artery calcium in young persons with
diabetes. 7: 241-247
(288) J Nucl Cardiol 2014; Paixao AR, Berry JD. Beyind Framingham
and coronary calcium: predicted lifetime risk identifies
unfavorable risk trajectories. 21: 42-45
(289) J Nucl Cardiol 2014; Nasir K, Blaha MJ. Short and lifetime
cardiovascular risk estimates: same wine, different bottles. Do we
have the COURAGE to abandon risk scores? 21: 46-49
(290) J Cardiovasc Comput Tomogr
2014; Kondo T, et al. Motion artifacts on coronary CT
angiography images in patients with a pericardial effusion. 8:
19-25
(291) J Cardiovasc Comput Tomogr 2014; Patel J, et al.
All-cause mortality in asymptomatic persons with extensive
Agatston scores above 1000. 8: 26-32
(292) J Cardiovasc Comput Tomogr 2014; Aslam A, et al.
Assessment of isotropic calcium using 0.5-mm reconstructions
from 320-row CT data sets identifies more patients with non-zero
Agatston score and more subclinical atherosclerosis than
standard 3.0-mm coronary artery calcium scan and CT angiography.
8: 58-66
(293) J Cardiovasc Comput Tomogr 2014; Celik O, et al.
Comparison of different strategies of ivabradine premedication
for heart rate reduction before coronary computed tomography
angiography. 8: 77-82
(294) J Nucl Cardio 2014; Shah S, et
al. Prognostic significance of calcified plaque among
symptomatic patients with nonobstructive coronary artery
disease. 21: 453-466
(295) Radiographics 2014;
Litmanovich DE, et al. Dose reduction in cardiothoracic CT: review
of currently available methods. 34: 1469-1489
(296) Radiology 2014; Willemink MJ, et al. Coronary artery
calcification scoring with state-of-the-art CT scanners from
different vendors has substantial effect in risk classification.
273: 695-702
(297) AJR 2015; Galperin-Aizenberg M, et al. Cardiac CT
angiography in the emergency department. 204: 463-474
(298) Radiology 2015; Puchner SB, et al. High-risk coronary
plaque at coronary CT angiography is associated with nonalcoholic
fatty liver disease, indpendent of coronary plaque and stenosis
burden: results from the ROMICAT II trial. 274: 693-701
(299) J Cardiovasc Comput Tomogr 2015; Alluri K, et al.
Distribution and burden of newly detected coronary artery calcium:
results from the mutli-ethnic study of atherosclerosis. 9: 337-344
(300) Radiographics 2015; Machida H, et al. Current and novel
imaging techniques in coronary CT. 35: 991-1010
(301) J Nucl Cardiol 2016; van den Hoogen IJ, et al. Prognostic
value of coronary computed tomography in diabetic patients without
chest pain sysndrome. 23: 24-36
(302) J Cardiovasc Comput Tomogr 2016; Nadjiri J, et al.
Incremental prognostic value of quantitative plaque assessment in
coronary CT angiography during 5 years of followup. 10: 97-104
(303) J Cardiovasc Comput Tomogr 2016; Hell MM, et al Epicardial
adipose tissue volume but not density is an independent predictor
for myocardial ischemia. 10: 141-149
(304) J Cardiovasc Comput Tomogr 2016; Takahashi M, et al.
Comparison of adaptive statistical iterative and filtered back
projection reconstruction techniques in quantifying coronary
calcium. 10: 61-68
(305) J Nucl Cardiol 2016; Cantoni V, et al. Long-term prognostic
value of stress myocardial perfusion imaging and coronary computed
tomography angiography: a meta-analysis. 23: 185-197
(306) J Nucl Cardiol 2016; Naya M, Tamaki N. Stress MPI, coronary
CTA, and multimodality for subsequent risk analysis. 23: 198-201
(307) J Cardiovasc Comput Tomogr 2016; Sekimoto T, et al.
Regional calcified plaque score evaluated by mutlidetector
computed tomography for predicting the addition of rotational
atherectomy during percutaneous coronary intervention. 10: 221-228
(308) J Nucl Cardiol 2016; Berman DS, Rozanski A. Value-based
imaging: combining coronary artery calcium with myocardial
perfusion imaging. 23: 939-941
(309) J Cardiovasc Comput Tomogr 2016; Schuhnaeck A, et al.
Influence of coronary calcium score on the ability to rule out
coronary artery stenoses by coronary CT angiorgaphy in patients
with suspected coronary artery disease. 10: 343-350
(310) J Nucl Cardiol 2017; Assante R, et al. Quantitative
relationship between coronary artery calcium and myocardial blood
flow by hybrid rubidium-82 PET/CT imaging in patients with
suspected coronary artery disease. 24: 494-501
(311) J Nucl Cardiol 2017; Rozanski A, et al. Use of coronary
artery calcium scanning as a triage for cardiac ischemia testing.
24: 502-506
(312) J Nucl Cardiol 2017; Engbers EM, et al. Coronary artery
calcium score as a gatekeeper in the non-invasive evaluation of
suspected coronary artery disease in symptomatic patients. 24:
826-831
(313) Radiology 2018; Pazhenkottil AP, et al. Hybrid SPECT
perfusion imaging and coronary CT angiography: long-term
prognostic value for cardiovascular outcomes. 288: 694-702