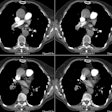
Pulmonary Vein Stenosis
Clinical:
Congenital pulmonary vein stenosis usually involves multiple veins bilaterally with varying degrees of stenosis. There is no predilection for either side [5]. The embryologic mechanism leading to the stenosis is unknown. The stenotic regions are located at the junction of the pulmonary veins and the left atrium. The condition usually manifests with pulmonary sympomts during the first 3 years of life [5]. Prognosis is poor (unless there is stenosis of a solitary pulmonary vein which is usually well tolerated [4])- there is no medical therapy available and surgical intervention or balloon dilatation is often not effective.
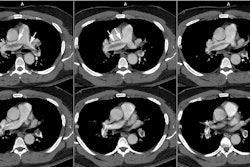
Pulmonary vein stenosis can occur following radiofrequency ablation for atrial fibrillation [3]. In most individuals, the sleeves of the left atrial myocardium extend into the pulmonary veins for a distance between 2mm to 17 mm and may cause ectopic electric activity [3]. Over 90% of ectopic beats that lead to atrial fibrillation originate in the pulmonary veins and almost half occur in the left superior pulmonary vein [3]. Radiofrequency ablation can eliminate atrial fibrillation in more than 70% of patients [3]. A mild venous stenosis secondary to thermal injury is found in more than 40% of patients following the procedure [3]. When more than 30W of power are used during the procedure, severe venous stenosis can result [3]. Venous thrombosis and venous infarctions can also occur [3]. Pulmonary vein stenosis is usually treated with angioplasty or stent placement (although angioplasty alone has a high failure rate and restenosis) [5].
X-ray:
The radiographic findings depend upon the number of vessels involved, their distribution, and the degree of stenosis. Findings may include a small lung, regional asymmetric vascularity, and reticular opacities with Kerley lines [5]. On angiography, there is asynchronous filling of the constricted pulmonary veins.
Pulmonary Vein Atresia:
Clinical:
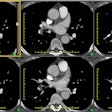
Unilateral pulmonary vein atresia is a rare anomaly that likely
results from failure of
incorporation of the common pulmonary vein into the left atrium
[2]. It
may occur in
either lung, with no right- or left-sided predominance [2].
Affected
patients usually
present in infancy or childhood with recurrent episodes of
pneumonia or
hemoptysis (due to
systemic collateral supply to the affected lung) [2]. Associated
congenital heart defects
are found in about 50% of patients [2].
Atresia of the common pulmonary vein is a rare anomaly thought to
be
due to failure of the CPV to establish connection to the left
atrium or
to regression of the connection following its establishment [4].
The
defect occurs at a later stage than patients who develop TAPVR
[4].
Unlike TAPVR, there is no vascular channel returning the blood to
the
right atrium and the intraparenchymal pulmonary veins are
underdeveloped [4]. Small collateral veins serve to decompress
pulmonary venous blood to other systemic channels [4]. The
condition
manifests in the neonatal period with extreme cyanosis from
pulmonary
venous obstruction [4]. The condition is often fatal and surgical
palliation is difficult due to the absence of well-pdeveloped
pulmonary
veins [4].
X-ray:
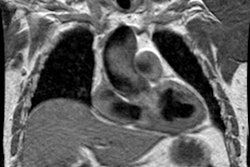
The ipsilateral hemithorax is small and there are unilateral reticular opacities with septal (Kerly) lines and peribronchovascular thickening. The ipsilateral pulmonary arteries are generally hypoplastic [2].
REFERENCES:
(1) Seminars in Roentgenology 1989; Budorick NE, et al. The pulmonary veins. 24 (2) Apr: 127-140 (Review. No abstract available.)
(2) AJR 2001; Heyneman LE, et al. Congenital unilateral pulmonary vein atresia: Radiologic findings in three adult patients. 177: 681-685
(3) AJR 2002; Ravenel JG, McAdams HP. Pulmonary venous infarction
after
radiofrequency ablation for atrial fibrillation. 178: 664-666 (No
abstract
available)
(4) Radiographics 2012; Vyas HV, et al. MR imaging and CT
evaluation
of
congenital pulmonary vein abnormalities in neonates and infants.
32:
87-98
(5) Radiographics 2013; Porres DV, et al. Learning from the
pulmonary veins. 33: 999-1022