J Nucl Med 2002 Jun;43(6):811-27
Radioguided sentinel lymph node biopsy in malignant cutaneous melanoma.
Mariani G, Gipponi M, Moresco L, Villa G, Bartolomei M, Mazzarol G, Bagnara MC,
Romanini A, Cafiero F, Paganelli G, Strauss HW.
The procedure of sentinel lymph node biopsy in patients with malignant cutaneous
melanoma has evolved from the notion that the tumor drains in a logical way
through the lymphatic system, from the first to subsequent levels. As a
consequence, the first lymph node encountered (the sentinel node) will most
likely be the first affected by metastasis; therefore, a negative sentinel node
makes it highly unlikely that other nodes in the same lymphatic basin are
affected. Although the long-term therapeutic benefit of the sentinel lymph node
biopsy per se has not yet been ascertained, this procedure distinguishes
patients without nodal metastases, who can avoid nodal basin dissection with its
associated risk of lymphedema, from those with metastatic involvement, who may
benefit from additional therapy. Sentinel lymph node biopsy would represent a
significant advantage as a minimally invasive procedure, considering that an
average of only 20% of melanoma patients with a Breslow thickness between 1.5
and 4 mm harbor metastasis in their sentinel node and are therefore candidates
for elective lymph node dissection. Furthermore, histologic sampling errors
(amounting to approximately 12% of lymph nodes in the conventional routine) can
be reduced if one assesses a single (sentinel) node extensively rather than
assessing the standard few histologic sections in a high number of lymph nodes
per patient. The cells from which cutaneous melanomas originate are located
between the dermis and the epidermis, a zone that drains to the inner lymphatic
network in the reticular dermis and, in turn, to larger collecting lymphatics in
the subcutis. Therefore, the optimal route for interstitial administration of
radiocolloids for lymphoscintigraphy and subsequent radioguided sentinel lymph
node biopsy is intradermal or subdermal injection. (99m)Tc-Labeled colloids in
various size ranges are equally adequate for radioguided sentinel lymph node
biopsy in patients with cutaneous melanoma, depending on local experience and
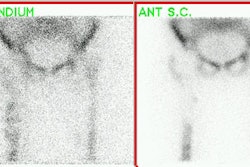
availability. For melanomas along the midline of the head, neck, and trunk,
particular consideration should be given to ambiguous lymphatic drainage, which
frequently requires interstitial administration virtually all around the tumor
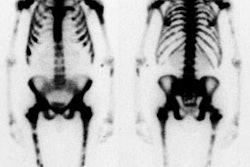
or surgical scar from prior excision of the melanoma. Lymphoscintigraphy is an
essential part of radioguided sentinel lymph node biopsy because images are used
to direct the surgeon to the sites of the nodes. The sentinel lymph node should
have a significantly higher count than that of the background (at least 10:1
intraoperatively). After removal of the sentinel node, the surgical bed must be
reexamined to ensure that all radioactive sites are identified and removed for
analysis. Virtually the entire sentinel lymph node should be processed for
histopathology, including both conventional hematoxylin-eosin staining and
immune staining with antibodies to the S-100 and HMB-45 antigens. The success
rate of radioguidance in localizing the sentinel lymph node in melanoma patients
is approximately 98% in institutions that perform a high number of procedures
and approaches 99% when combined with the vital blue-dye technique. Growing
evidence of the high correlation between a sentinel lymph node biopsy negative
for cancer and a negative status for the lymphatic basin-evidence, therefore, of
the high prognostic value of sentinel node biopsy-has led to the procedure's
being included in the most recent version of the TNM staging system and starting
to become the standard of care for patients with cutaneous melanoma.