Dynamic chest radiography is a promising new tool for diagnosing patients with breathing symptoms related to diaphragm dysfunction, according to a study published February 21 in European Respiratory Journal (ERJ) Open Research.
In a pilot study, U.K. investigators explored the use of dynamic chest radiography in a series of patients with symptoms suggesting diaphragm dysfunction. The technique provided promising real-time metrics on diaphragm and chest wall motion and warrants further study to see if it can complement established tools, such as ultrasound and traditional fluoroscopy, the authors suggested.
"[Dynamic chest radiography], which combines the visual ease of fluoroscopy with the ability to provide quantifiable measures of hemidiaphragm and chest wall movement, may be of use as an adjunct technique," wrote corresponding author Dr. Thomas FitzMaurice of the University of Liverpool's Heart and Chest Hospital.
Dynamic chest radiography is a novel real-time digital fluoroscopic imaging system that produces clear, wide field-of-view diagnostic images of the thorax and diaphragm in motion, alongside novel metrics on moving structures within the thoracic cavity.
Previous studies have shown the technique can be used to assess average movement of the diaphragm during tidal and deep breathing in healthy volunteers, as well as abnormal diaphragm dynamics in people with severe chronic obstructive pulmonary disorder.
In this study, FitzMaurice and colleagues tested the technique for visualizing diaphragm motion in a series of patients with suspected damage of the phrenic nerve, which controls the diaphragm and, ultimately, normal breathing.
The group enrolled 21 consecutive patients referred for diaphragm function testing based on suspicious plain chest x-rays, clinical symptoms (breathlessness, orthopnea, reduced exercise tolerance), and/or suggestive history (cardiac intervention, trauma, or infection).
Imaging was performed using a dynamic radiography system from Konica Minolta Healthcare for cineradiographic imaging and installed in a standard radiography room.
Patients were instructed to take three sharp sniffs followed by a breath to full inspiration then full expiration. Images were acquired in the posteroanterior plane, in a standing position, with a maximum allowable image exposure time of 300 frames, or 20 seconds.
The researchers observed paradoxical motion (in which the diaphragm moves in the opposite direction than it should during inhaling and exhaling) in 14 patients, and they confirmed it in six who also underwent fluoroscopy or ultrasound. In four patients, dynamic chest radiography showed reduced hemidiaphragm excursion, but no paradoxical motion. In three patients, the researchers observed normal diaphragm motion.
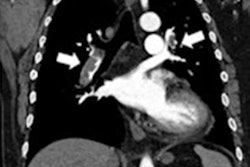
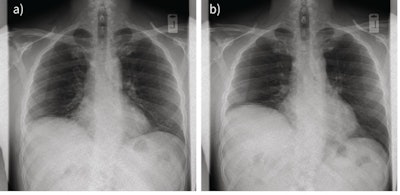 Two still images from a dynamic chest radiography sequence showing paradoxical movement of the paralyzed right hemidiaphragm from (a) rest to (b) end sniff maneuver. Image courtesy of ERJ Open Research.
Two still images from a dynamic chest radiography sequence showing paradoxical movement of the paralyzed right hemidiaphragm from (a) rest to (b) end sniff maneuver. Image courtesy of ERJ Open Research.In addition, the time taken for preparation, patient instruction, and image acquisition was approximately five minutes per patient, which is comparable to standard chest x-rays, the authors noted.
"Here, [dynamic chest radiography] proved quick and straightforward to perform," they wrote. "It produces easily interpretable metrics on diaphragm and chest wall motion that warrant further study alongside established diagnostic tools."
Possible advantages of digital chest radiography over ultrasound or fluoroscopy include shorter acquisition times, with visual results available to the ordering clinician immediately after acquisition, and at a lower radiation dose than fluoroscopy, FitzMaurice et al suggested.
In addition, dynamic MRI has been used as a tool to analyze diaphragm function, but it is typically not used in clinics due to its high cost, limited availability, and separate MRI suite. On the other hand, the small footprint of digital chest radiography could allow installations in standard radiography rooms, the authors added.
"To our knowledge, this is the first time [dynamic chest radiography] has been used in the investigation of hemidiaphragm dysfunction, and there remains large potential for further work," the group concluded.