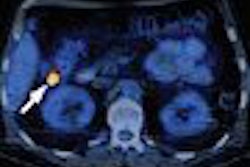
Overall, dark-lumen MR colonography (MRC) does a good job of detecting sigmoid diverticulitis, researchers from University Hospital in Essen, Germany, concluded in the online edition of European Radiology. But their study revealed some shortcomings of MRC as well, notably its inability to differentiate between colon cancer and diverticular disease.
Diverticular disease is common in the West, an unfortunate result of too many low-fiber diets in fast-food nations. Moreover, good methods of detecting the disease are as hard to come by as brown rice at a Burger King.
CT has high spatial resolution, for example, but tortuous colons can make CT colonography (virtual colonoscopy) data difficult to interpret in the presence of diverticular disease. Conventional colonoscopy can be stopped by stenosis before it reaches the cecum.
The barium enema is getting harder to obtain, and is prone to low sensitivity. The exam is also contraindicated in cases of acute diverticulitis or suspected perforation due to the potential risk of developing peritonitis. Transabdominal ultrasound, which the authors cite as another potentially useful tool in patients with diverticular disease, can miss perforations and abscesses, and cannot assess the colonic wall segments proximal to the area of diverticulitis.
"In suspected acute diverticulitis, a reliable imaging technique is needed for the initial therapeutic decision as to whether to employ medical or surgical treatment, because clinical data or laboratory parameters are frequently inconclusive or unspecific," wrote Drs. Waleed Ajaj, Stefan G. Ruehm, Thomas Lauenstein, Susanne Goehde, Christiane Kuehle, Christoph Herborn, and colleagues from the University Hospital in Essen, Germany; Medical Center Hamburg-Eppendorf in Hamburg, Gemany; and the University of California, Los Angeles (European Radiology, August 13, 2005).
Diverticulitis (generally defined as an extramucosal inflammation with wall thickening) of the right colon is the most common colonic disease in Western countries, affecting 10% to 50% of those older than age 60, the researchers noted. Patients with a history of diverticular disease are subject to recurrence at a risk of 7% to 35%.
The study consisted of 40 patients (24 women, 16 men; age range 55-77 years) with suspected diverticular disease. The group sought to determine the appropriateness of dark-lumen MRC as a method of detecting sigmoid diverticulitis. All patients underwent MRC within 72 hours before conventional colonoscopy.
"Beyond the clinical suspicion, patients exhibited high inflammatory parameters (leukocytosis > 13,000/nl and/or C-reactive protein 1.5 mg/dl, and clinical symptoms such as abdominal pain, pararectal bleeding, fever, and diarrhea," they wrote.
Before imaging, the patients underwent standard bowel cleansing with 3,000 mL of a polyethylene glycol solution (Golytely, Braintree Laboratories, Braintree, MA), at a dose of 2,000 mL the night before imaging and 1,000 mL the day of the exam. To minimize peristaltic movement, 40 mg of scopolamine (Buscopan, Boehringer Ingelheim, Ingelheim, Germany) was injected prior to imaging. Finally, the colon was filled with approximately 2000-2500 mL of warm tap water to patient tolerance.
Patients were then scanned only in the prone position. MRI was performed in a single breath-hold (approximately 22 seconds) on a 1.5-tesla scanner (Magnetom Sonata, Siemens Medical Solutions, Erlangen, Germany), using two surface coils in conjunction with a spine-array coil. T1-weighted 3D gradient-echo data were acquired in the coronal plane at TR/TE 3.1/1.1 msec, flip angle of 12 degrees, 450 x 450 mm field-of-view, 168 x 256 matrix, 96 slices, and 1.6-mm slice thickness. The same imaging parameters were repeated 75 seconds after intravenous injection of a paramagnetic contrast agent (gadobenate dimeglumine, MultiHance, Bracco, Milan, Italy).
Colonoscopy was performed within 72 hours of MRC, and the gastroenterologist was unaware of the MRI findings, Ajaj and colleagues wrote. In four cases the colonoscope failed to reach the cecum due to stenosis.
Both the contrast and noncontrast MRC datasets were examined on a postprocessing workstation (Virtuoso, Siemens Medical Solutions), where they were analyzed by two experienced gastrointestinal radiologists. MR image quality was sufficient for diagnosis in all patients.
According to the results, 17 of the 40 patients were found to be normal with regard to sigmoid diverticulitis at MRC. In four of these patients, however, colonoscopy confirmed the presence of light inflammation. MRC correctly identified wall thickness and contrast uptake in the sigmoid colon in the remaining 23 patients.
Of these 23 patients, four were found to have a high-grade stenosis of the sigmoid colon, and five other patients had pericolic abscesses. In five patients, MRC also detected six colorectal lesions ranging from 6-15 mm. However, three cases that were positive for diverticular disease at MRC were deemed false-positive at colonoscopy, the authors wrote.
In another three of the 23 cases, MRC classified the inflammation as diverticulitis, whereas conventional colonoscopy and histopathology confirmed the presence of invasive carcinoma.
Extracolonic findings detected at MR colonography included multiple mesenteric lymph nodes in 12 patients, and liver and renal cysts and osteochodroses in 15.
"The findings presented here carry two messages we believe to be important: (a) MRC is accurate for the detection of sigmoid diverticulitis, and (b) MRC cannot differentiate between diverticulitis of the sigmoid colon," Ajaj and colleagues wrote.
"Schreyer et al examined 14 patients with clinically suspected diverticulitis examined by MRC using a 3D fast low-angle shot sequence. Having CT as a standard of reference, all sigmoid diverticula were diagnosed based on MRI. Inflammation as judged by CT was assessed identically on MRI (International Journal of Colorectal Disease, September 2004, Vol. 19:5, pp. 474-480).
CT has some advantages in terms of better spatial resolution, lower exam costs, and better scanner availability, the team noted. However, the safe contrast agents and lack of harmful side effects make MRI an attractive imaging option.
The present study, using a T1-weighted interpolated breath-hold acquisition, a water enema, and intravenous gadolinium-based contrast injection, is based on the focal uptake of contrast material in pathologies of colon wall.
"These pathologies are displayed as bright areas while the lumen is rendered totally dark due to water (dark-lumen MRC)" the team wrote."Based on wall thickness and contrast uptake, MRC has shown a sensitivity and specificity of 86% and 92%, respectively, for the detection of sigmoid diverticulitis."
Dark-lumen MRC can be considered an alternative to conventional colonoscopy for detecting sigmoid diverticulitis and other relevant pathologies of the colon, for example failed conventional colonoscopy, the authors concluded.
However, they added, "conventional colonoscopy accompanied by biopsy is necessary to exclude carcinoma in patients with sigmoid diverticulitis."
By Eric Barnes
AuntMinnie.com staff writer
September 19, 2005
Related Reading
VC, colonoscopy not optimal in patients with diverticular disease, May 25, 2005
Virtual colonoscopy's tortuous path in diverticular disease, June 20, 2002
Copyright © 2005 AuntMinnie.com