Fluoroscopy with a mini C-arm has the ability to manipulate, position, and image an injured wrist much more efficiently than conventional static radiography, according to a study presented at the 2009 American Academy of Orthopaedic Surgeons (AAOS) meeting in Las Vegas.
Researchers at Maimonides Medical Center in New York City made that conclusion in a direct comparison of the two modalities and their ability to accurately assess scapholunate diastasis, the space between the scaphoid and lunate. Co-author Dr. Philip Lahey, a second-year resident at Maimonides, collaborated on the paper with Dr. Jack Choueka, the chairman of Maimonides' department of orthopedics.
The study looked at 26 consecutive patients (15 women and 11 men), ranging in age from 31 to 78 years. "These patients had strains causing wrist pain for a variety of reasons, usually falls from an outstretched hand," Lahey said. "The specific diagnosis of a scapholunate tear was not made," he said, adding that there were no breaks or fractures among the patient's wrist injuries.
X-ray versus fluoro
With a standard x-ray, a technician will position a patient's wrist under the device to capture an angle that best reflects what a physician wants to view. While the wrist can be placed at different positions, Lahey describes the process as "sort of a guessing game" with many variables that can cause an inadequate image.
"The geometry and physiological variability of the wrist is such that everyone is a little bit different," he said. "Getting a straight-on view of the scaphoid and the lunate, so you can measure the space in between, is very difficult."
If the positioning of the wrist is off by even 10°, Lahey said, there may be just enough variation to place the two bones at an angle so the interval cannot be measured accurately. In addition, a patient may move inadvertently between positioning during the procedures; even moving fingers slightly can alter the intended view.
Radiation exposure
Also, with x-ray, radiation exposure "is such that you can't sit there and take x-ray after x-ray after x-ray trying to get the right view," Lahey added. "Even if you did try again, it would still be a guessing game in hopes you get the right angle this time."
By comparison, fluoroscopy via a mini C-arm is a low-intensity radiation x-ray, and a radiologic technologist can use a live image as a guide to move and rotate the wrist. "Fluoroscopy eliminates need for technician positioning and anatomical variations of the carpus, and allows the clinician to position the wrist in a manner that maximizes the scapholunate interval," the paper noted.
 |
| Dr. Jack Choueka used a mini C-arm to accurately position a patient's wrist for imaging the scapholunate interval. All images courtesy of Maimonides Medical Center. |
In the research, posteroanterior radiographs of both wrists, with and without grip views, were taken to determine the scapholunate interval. A clinician then used fluoroscopy to manipulate patients' wrists to obtain the maximum scapholunate distance with and without patient grip. Flouroscopic images were digitized for measurement and a radiographic ruler was used for calibration.
In the review of 26 patients, the researchers found that an overlap of the scaphoid and lunate, which prevented measuring the scapholunate interval, occurred in 13% (14 of 104) of all plain radiographs taken. There was no overlap in the fluoroscopic images.
Fluoroscopy also was able to reveal a scapholunate space greater than 2 mm in the wrists, while only 28% (five of 18 wrists) of plain radiographs displayed a scapholunate space greater than 2 mm. The average space measured by plain radiographs was 1.23 mm, compared with 2.23 for fluoroscopy.
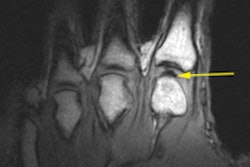
 |
| The two clinical images show the difference in a plain radiograph (above) and fluoroscopic image (below) of the same wrist and the modalities' ability to show the scapholunate interval. |
 |
The 2-mm benchmark is important because if the scapholunate space, or interval, is greater than 2 mm, the wrist injury requires additional follow-up. "It doesn't automatically mean the scapholunate or the ligament is torn," Lahey said, "but if [the scapholunate space] is greater than 2 mm and it is different than the other side -- the contralateral wrist -- then it warrants further investigation and most likely is torn."
As for the use of fluoroscopy and C-arms with other joints, such as ankles and elbows, Lahey said that the modality may be useful in some cases.
Although it is more common for physicians to have a mini C-arm in an outpatient setting, Lahey said previous research has not described fluoroscopy "as the definitive tool" for all joint imaging. "There is some expense associated with [a mini C-arm], but it may show that it is worth having it in an office," he added.
By Wayne Forrest
AuntMinnie.com staff writer
February 26, 2009
Related Reading
3-tesla MRI effective in wrist tear detection, January 9, 2009
MRI, US far from idle for hand, wrist injuries, November 6, 2006
MRI, x-ray yield comparable sensitivities for RA joint erosion, June 10, 2005
The twists and turns of hand and wrist x-ray positioning, October 15, 2002
Digit imaging requires diligent positioning, September 17, 2002
Copyright © 2009 AuntMinnie.com