Restricting the daily use of chest x-rays in intensive care units (ICUs) reduces the cost associated with delivering care without a concomitant increase in complications, according to research published in the March issue of the Journal of the American College of Radiology.
Researchers led by Dr. Jinel Scott of Kings County Hospital Center in New York City changed the exam ordering practices in their adult ICUs to align with established evidence-based guidelines, reducing the use of portable chest x-rays by 37%. There was no concomitant increase in unplanned extubations or ventilator days.
Implementing the study model could safely save the hospital system up to $5 million over the next 10 years, the researchers suggested.
"The value radiology departments bring to institutions should extend beyond image interpretation. Both radiology leadership and frontline staff members should take a central role in implementing already established, evidence-based practices in imaging," they wrote (JACR, March 2021, Vol. 18:3, pp. 354-360).
Daily chest x-ray remains standard practice at many institutions, despite the American College of Radiology's recommendation against the practice. In the current study, a multidisciplinary performance improvement team set out to reduce portable chest radiographs in adult ICUs by 5% between June and December 2019. They eliminated standing orders for chest x-ray, changed workflow, and implemented an education campaign that targeted residents and critical care attending physicians.
A hard stop preventing the routine ordering of chest x-rays could not be deployed within the electronic health record (EHR) system, the authors noted, so adherence to the new workflow and practices relied heavily on continuous education and feedback. They emphasized that a daily chest x-ray rarely changes patient management and that there are significant disadvantages associated with the practice, including radiation exposure, sleep disturbances, equipment dislodgement, and skin shear injuries from positioning maneuvers.
Instead of routine orders, the need for a chest x-ray was determined only after examining the patient or on the basis of clinical events such as placement of a line, desaturation, or fever.
The authors noted that house staff education was a particular challenge because each month brought a new cohort of residents and interns. Weekly email reminders were sent to residents, and faculty members were tasked with emphasizing the new approach to patient care during rotation orientation and reemphasizing these strategies in daily rounds. In addition, visual cues deployed at workstations served as reminders of the new, more restrictive, event-driven approach to ordering radiographs.
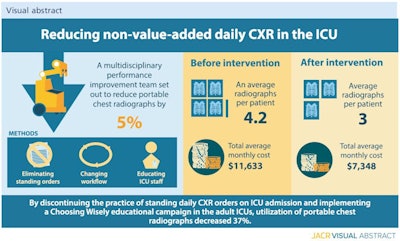 Curbing daily use of chest x-ray in ICU cuts major costs. Image courtesy of the JACR.
Curbing daily use of chest x-ray in ICU cuts major costs. Image courtesy of the JACR.Prior to the intervention, an average of 4.2 x-rays were performed per patient at a total average monthly cost of $11,633. After the intervention, the average number of x-rays per patient dropped to three for a total average monthly cost of $7,348. By using time-driven activity-based costing (TDABC) principles, the researchers determined the restrictive model could potentially save their institution about $4,000 a month, or $48,000 annually. Throughout the system, that could add up to a savings of $5 million over the next 10 years.
The authors noted that the impact of COVID-19 on this initiative has yet to be fully determined. There was no time to thoroughly orient and educate new teams on all the ICU practices. As a result, some physicians may have ordered unwarranted daily chest x-rays.
However, in addition to the already established benefits, a restricted approach would have been the best approach during this crisis to decrease virus transmission to other patients, medical staff members, and radiologic technologists, they stated.
"This example affirms that the strongest intervention that would allow better sustainability in the long term would be a change in the EHR that prevents standing orders for daily [chest x-ray]," the authors concluded.