PET/MRI can better detect and classify local lesions and distant metastases in women suspected of having recurrent pelvic cancer than MRI alone, according to a study presented at the recent RSNA 2017 annual meeting.
Given PET/MRI's exact assessment of recurrence of female pelvic malignancies within their study, German researchers recommended that the hybrid modality should be considered a valuable alternative for whole-body staging of patients with suspected recurrent disease.
"As PET/MRI is able to detect markedly more malignant lesions than MRI alone and is also superior in the distinction of intrapelvic recurrence versus distant metastatic spread, it may help clinicians choose the optimal individual management strategy," said lead author Dr. Lino Sawicki, from the department of diagnostic and interventional radiology at the University of Düsseldorf.
Recurrence challenges
Pelvic cancers are among a heterogeneous group of neoplasms, most of which have a considerable risk of recurrence even after complete remission. While palliative therapy is the standard of care for the majority of women who experience recurrence, radical surgery may be the most appropriate option for some patients to eliminate the cancer.
 Dr. Lino Sawicki from the University of Düsseldorf.
Dr. Lino Sawicki from the University of Düsseldorf."Therefore, women with suspected relapse require precise restaging to aid clinicians and provide optimal care," Sawicki told RSNA attendees.
CT and ultrasound have been used in this patient population in the past, but both modalities have limited ability to distinguish between postoperative scar tissue and cancerous lesions, he noted. MRI, on the other hand, has proved effective for identifying local and distant recurrence of female pelvic cancers based on the higher soft-tissue contrast and the benefit of diffusion-weighted MR imaging.
"FDG-PET/MRI combines anatomic and functional details from the MR component with information on tissue vitality represented by glucose metabolism [on PET]," Sawicki explained. "There are also some comparative studies with PET/MRI that are very promising. However, there is only one pilot study comparing PET/MRI with MRI alone."
Thus, the aim of this study was to evaluate the diagnostic performance of FDG-PET/MRI compared with MRI alone for whole-body staging of women suspected of having recurrent pelvic cancer.
Modality comparison
The researchers retrospectively looked at 71 consecutive female patients with a mean age of 54 years (± 13 years). The subjects included 32 patients with recurrent cervical cancer, 26 cases of ovarian cancer, seven women with endometrial cancer, four patients with vulvar cancer, and two patients with vaginal cancer. All the women had undergone surgery and/or radiochemotherapy after initial cancer diagnosis and were cancer-free for six months or longer after treatment.
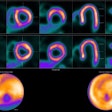
PET/MR imaging was conducted on an integrated device featuring a 3-tesla MRI system (Biograph mMR, Siemens Healthineers) from the skull base to the midthigh. Two radiologists independently interpreted the results in separate sessions four weeks apart to avoid any reading bias. Their analyses included the number of lesions, lesion location, and whether they were malignant or benign.
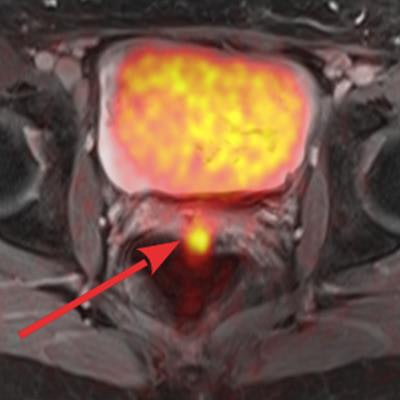
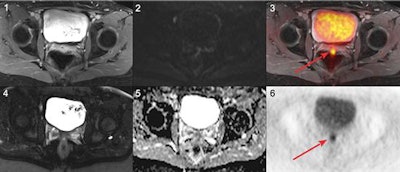 Images are from a 45-year-old woman with local recurrence of endometrial cancer. Postsurgical scar tissue is seen on a T1-weighted fast spin-echo (FSE) volumetric interpolated breath-hold examination (VIBE) (1) and T2-weighted FSE half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequence (4). PET (6) and PET/MR (3) images show a small focus of pathologically increased FDG uptake in the dorsal part of the scar tissue, indicating local relapse. No focal contrast enhancement or tumor was detectable on T1-weighted FSE VIBE (1) and T2-weighted FSE HASTE (4). The local recurrence did not exhibit a clearly focal restricted diffusion on diffusion-weighted MRI (2) and corresponding apparent diffusion coefficient map (5). Images courtesy of Dr. Lino Sawicki.
Images are from a 45-year-old woman with local recurrence of endometrial cancer. Postsurgical scar tissue is seen on a T1-weighted fast spin-echo (FSE) volumetric interpolated breath-hold examination (VIBE) (1) and T2-weighted FSE half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequence (4). PET (6) and PET/MR (3) images show a small focus of pathologically increased FDG uptake in the dorsal part of the scar tissue, indicating local relapse. No focal contrast enhancement or tumor was detectable on T1-weighted FSE VIBE (1) and T2-weighted FSE HASTE (4). The local recurrence did not exhibit a clearly focal restricted diffusion on diffusion-weighted MRI (2) and corresponding apparent diffusion coefficient map (5). Images courtesy of Dr. Lino Sawicki.The researchers used patients' histopathology data for reference standards. If histopathology results were not available, the researchers depended on follow-up imaging with a mean interval of eight months, a same-day PET/CT scan, and clinical follow-up.
Based on the reference standard, 55 patients (77%) experienced a cancer recurrence, while 16 patients (23%) had no such recurrence. PET/MRI correctly identified all 55 patients (100%) with cancer recurrence compared with MRI alone, which correctly identified 46 patients (83%) with cancer recurrence (p < 0.01). In addition, PET/MRI and MRI alone both correctly identified 15 (94%) of the 16 patients with no cancer recurrence.
In the lesion-based analysis, the reference standard identified 181 (75%) malignant lesions and 60 (25%) benign lesions. PET/MRI identified all malignant lesions, MRI alone discovered on 75%. As for the correct identification of benign lesions, PET/MRI (97%) and MRI were much more comparable (93%).
| Lesion-based analysis results | |||
| PET/MRI | MRI alone | p-value | |
| Malignant lesions | 181/181 (100%) | 135/181 (75%) | p < 0.001 |
| Benign lesions | 58/60 (97%) | 56/60 (93%) | p = 0.04 |
| Diagnostic accuracy | 99% | 79% | p < 0.001 |
While PET/MRI correctly identified all malignant lesions, the hybrid modality misclassified two foci of infection as malignant lesions. By comparison, MRI's missed 34 malignant lesions, which included 32 FDG-positive nonenlarged lymph node metastases. MRI alone also misinterpreted 12 malignant lesions as benign, which included four local recurrences and three peritoneal metastases.
Location, location
The researchers also divided patients into two groups based on the location of their recurrence: one set of subjects with recurrence limited to the pelvic cavity and a second set of patients with distant metastases.
Among the patients with recurrence in the pelvic cavity, PET/MRI identified all 15 patients (100%) compared with MRI alone, which correctly identified only 11 patients (73%) in this category. Among patients with distant metastases, PET/MRI correctly identified all 40 patients (100%), compared with 32 correctly identified patients (80%) by MRI alone.
"We found that in staging of women with recurrent pelvic cancer hybrid imaging with PET/MRI is significantly superior both on a per-patient and per-lesion basis, as compared with MRI alone," Sawicki concluded. "We also found that PET/MRI enables statistically significant classification of patients with local versus patients with distant metastases spread, thus potentially improving therapy planning."
Results from this study are not entirely surprising, Sawicki told AuntMinnie.com, given that previous research on the role of PET/MRI for staging or recurrent gynecologic pelvic cancers has indicated very high diagnostic performance of PET/MRI, compared with conventional imaging such as CT or MRI.
"But being a follow-up study comprising a larger patient cohort, the current data add validity to these prior results and further propagate hybrid imaging in terms of PET/MRI for imaging of recurrent female pelvic malignancies," he added.