Tau PET scans can help diagnose Alzheimer's disease on top of extensive clinical work-ups in participants with cognitive symptoms, according to a study published May 22 in JAMA Neurology.
Researchers led by Dr. Ruben Smith, PhD, of Skåne University Hospital in Lund, Sweden, found that including tau PET in the diagnostic work-up of a large group of memory clinic patients resulted in a change in diagnosis and a change in medication in a significant number.
"Before widespread implementation of tau PET as a diagnostic method in the clinic, it is vital to establish if the method shows an added clinical value for diagnosis and treatment," the researchers wrote.
In what is described as the "cascade hypothesis," Alzheimer disease is believed to be caused by the accumulation of beta amyloid in the brain followed by a gradual spread of tau as clinical symptoms emerge. PET radiotracers that visualize both beta-amyloid and tau protein have been developed that allow doctors to visualize this activity.
In this study, the Swedish group performed PET scans using F-18 RO948 radiotracer (which is being tested in late-stage clinical trials in Europe) in 878 memory clinic patients who had already undergone a clinical examination, cognitive testing, a brain MRI, and relevant testing for cerebrospinal fluid markers. Based on this workup, 408 patients had an Alzheimer's disease diagnosis and 470 did not.
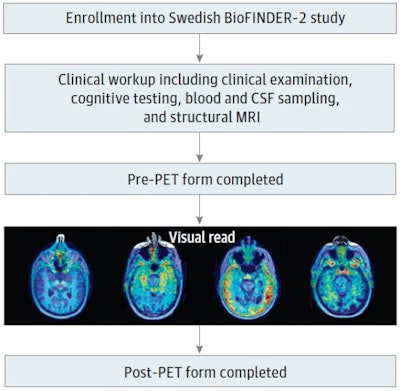 Patients with memory complaints were recruited to the study after a comprehensive clinical workup, including clinical examination, cognitive testing, structural imaging MRI, and blood/cerebrospinal fluid sampling. The clinician filled out the pre-PET form, indicating diagnosis, suspected underlying etiology, certainty of etiology, and treatment. The clinician then received the outcome of the visual read and filled out the post-PET form. Image courtesy of JAMA Neurology through CC BY 4.0.
Patients with memory complaints were recruited to the study after a comprehensive clinical workup, including clinical examination, cognitive testing, structural imaging MRI, and blood/cerebrospinal fluid sampling. The clinician filled out the pre-PET form, indicating diagnosis, suspected underlying etiology, certainty of etiology, and treatment. The clinician then received the outcome of the visual read and filled out the post-PET form. Image courtesy of JAMA Neurology through CC BY 4.0.Subsequent tau PET imaging led to a change in the diagnosis of 7.5% of the total population, according to the findings. In patients with a pre-PET diagnosis, 11.5% of cases were changed to a non-Alzheimer's diagnosis after the scans, and 4% of those with a pre-PET nondiagnosis were changed to a post-PET diagnosis.
In addition, changes in cognitive or antidepressant medication were made in 48 participants of the total population (5.5%) after the tau PET exams, the researchers added.
"We found that increased [Alzheimer's disease] diagnosis certainty was associated with tau PET in participants where [Alzheimer's disease] was the primary suspected pre-PET etiology, irrespective of cognitive status," the group wrote.
Ultimately, with promising new treatments for Alzheimer's disease under development, increasing diagnostic certainty is becoming more important, the group noted, and to that end, they recommended the clinical use of tau PET in patients with abnormal beta-amyloid pathology.





















