PET/MRI can provide high diagnostic performance for restaging gynecological cancer patients compared with FDG-PET/CT, with only slightly longer scan time and "markedly reduced" radiation exposure, according to a German study published online in the European Journal of Radiology.
Lead author Dr. Johannes Grueneisen and colleagues from University Hospital Essen and University Hospital Dusseldorf found no significant differences between the two hybrid modalities in terms of sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy.
 Dr. Johannes Grueneisen from University Hospital Essen.
Dr. Johannes Grueneisen from University Hospital Essen.The researchers used a first postcontrast subtracted, or FAST, imaging protocol, which consisted of a whole-body diffusion-weighted echo-planar imaging (EPI) sequence, a half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequence, and a postcontrast 3D volumetric interpolated breath-hold examination (VIBE) sequence.
The results suggest that PET/MRI with FAST could be a viable alternative for the diagnostic workup of patients with gynecological cancer, the group concluded.
Important benefits
PET/MRI has been touted in previous research for its accurate assessment of cancer patients by combining simultaneous whole-body PET with whole-body MRI. MRI's benefits include superior soft-tissue contrast with less ionizing radiation exposure than CT.
In fact, the current study follows another one by Grueneisen et al in which PET/MRI provided "significantly higher lesion contrast and diagnostic confidence in the detection of malignant lesions compared to MRI alone" (Investigative Radiology, December 2014, Vol. 49:12, pp. 808-815).
However, PET/MRI does suffer from longer scan time due to the need for additional MRI sequences.
"Hence, with regard to patient comfort, well-considered and suitable MR imaging protocols are required," they wrote.
In this study, Grueneisen and colleagues retrospectively analyzed 24 women with a mean age of 57 ± 13 years (range, 27-74 years). Thirteen women had ovarian cancer, seven had cervical cancer, and four had endometrial cancer as a primary diagnosis. Based on the follow-up imaging reference standard, 21 (88%) of the 24 patients had tumor recurrence (EJR, August 19, 2015).
Imaging protocols
Whole-body PET/CT exams included CT (Biograph mCT 128, Siemens Healthcare) approximately 70 seconds after intravenous administration of 100 mL of iodinated contrast (Ultravist 300, Bayer HealthCare Pharmaceuticals). PET images were acquired from the skull base to the upper thigh in five to seven bed positions of two minutes each.
Whole-body FAST PET/MRI exams were performed simultaneously on a 3-tesla MRI scanner (Biograph mMR, Siemens) using a dedicated mMR head-and-neck coil and phased-array body surface coils. Scanning began an average of 132 ± 25 minutes after FDG injection. PET scans spanned the skull base to the midthigh in four to five bed positions of eight minutes each.
Total scan time for the FDG-PET/CT scan was 18 ± 1 minutes, compared with 27.5 ± 2 minutes for the FAST PET/MRI protocol.
Two board-certificated radiologists who were blinded to the patients' data and diagnosis analyzed the PET/CT and PET/MRI results separately. There was a four-week interval between the readings to avoid any recognition bias.
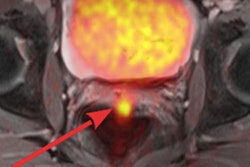
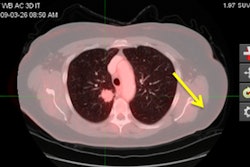
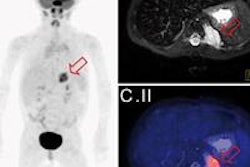
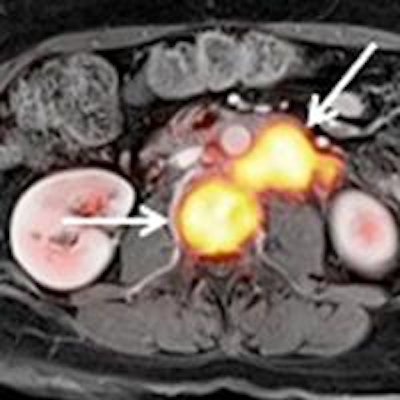
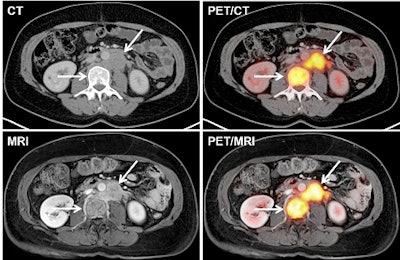 Images of a patient with a recurrence of cervical cancer. CT and MRI show a para-aortic lymph node metastasis and bone metastasis (arrows), which disclose pathological glucose metabolism on fused PET/CT and PET/MR images. Courtesy of Dr. Johannes Grueneisen.
Images of a patient with a recurrence of cervical cancer. CT and MRI show a para-aortic lymph node metastasis and bone metastasis (arrows), which disclose pathological glucose metabolism on fused PET/CT and PET/MR images. Courtesy of Dr. Johannes Grueneisen.Lesion detection
PET/CT and PET/MRI correctly identified tumor relapse in 20 (95%) of the 21 patients. For the other three patients, PET/MRI had one false-positive result, whereas PET/CT correctly classified all three patients as having no tumor recurrence.
The reference standard detected a total of 104 suspicious lesions, of which 81 (78%) were malignant and 23 (22%) were benign. The researchers found no significant differences between the two hybrid modalities in terms of lesion detection (p > 0.05)
| Detection of malignant lesions | ||
| Measurement | PET/CT | PET/MRI |
| Sensitivity | 82% | 85% |
| Specificity | 91% | 87% |
| Positive predictive value | 97% | 96% |
| Negative predictive value | 58% | 63% |
| Diagnostic accuracy | 84% | 86% |
In terms of qualitative assessment for visualizing lesions, PET/CT showed significantly higher values for the delineation of lung metastases, while PET/MRI achieved significantly higher lesion-to-background contrast for bone metastases.
"Our study results demonstrate the feasibility and high diagnostic value of the applied FAST PET/MRI protocol for restaging female patients suspect for a recurrent pelvic malignancy," Grueneisen and colleagues concluded. "Furthermore, the implementation of a FAST PET/MRI protocol enables high-quality restaging of gynecological cancer patients within only slightly longer scan duration in comparison to PET/CT."
The authors highlighted the benefits of PET/MRI, noting its "excellent soft-tissue contrast" and "markedly reduced radiation exposure" compared to full-dose FDG-PET/CT.
"This is of particular importance considering repetitive examinations for follow-up imaging of cancer patients, especially for a younger patient population and/or tumor entities that are associated to low mortality rates," they wrote.
The researchers cited several limitations of their study, including its retrospective approach and the limited number of patients who met the inclusion criteria.
"Therefore, our results should be considered as preliminary and the investigation of larger patient cohorts should be the focus of further prospective trials," they wrote.
They also noted that the FAST MRI technique is based on a selection of previously obtained prolonged examination protocols.
"Hence, the clinical feasibility of an exclusive FAST PET/MRI for restaging gynecological cancer patients should be investigated in future studies," they added.