Young pediatric patients may benefit from FDG-PET/MRI for staging and clinically evaluating oncologic disorders, given the hybrid modality's superior soft-tissue contrast and significantly lower radiation dose, according to a study published online August 24 in Investigative Radiology.
German researchers found FDG-PET/MRI to be at least as good as FDG-PET/CT for evaluating pediatric cancer patients younger than 6 years, potentially changing the treatment plan for almost half of the study's cohort.
"These advantages of MRI were observed despite the fact that we only used noncontrast-enhanced MRI in our study due to ethical restrictions," wrote the team led by Dr. Sergios Gatidis from the University of Tübingen. "The addition of contrast-enhanced MRI may further substantially increase diagnostic performance, especially concerning lesion characterization and interpretation."
Focus on younger patients
Children younger than 6 offer unique challenges for radiologists. Repeated scans, particularly with CT, may result in radiation-induced malignancies. In addition, these patients have difficulty remaining still for PET/CT or PET/MRI exams, which can result in motion artifacts or the need for sedation (Invest Radiol, August 24, 2015).
Previous research has shown PET/MRI to be diagnostically equivalent to PET/CT for oncologic imaging, but those studies focused on adults or juvenile subjects, the authors wrote. Younger children have significantly different physiologic and anatomic characteristics.
 Dr. Sergios Gatidis from the University of Tübingen.
Dr. Sergios Gatidis from the University of Tübingen."Importantly, tumor entities in children are different from tumor entities observed in juveniles or adults," they wrote.
Gatidis and colleagues decided to investigate the value of PET/MRI in a study of six boys and three girls with a mean age of 4.8 years (range, 1-6 years). The subjects all had a proven or suspected solid malignant tumor and clinical indication for FDG-PET/CT.
PET/CT (Biograph mCT, Siemens Healthcare) and PET/MRI (Biograph mMR, Siemens) scans were performed sequentially within the same day using one injection of FDG. A total of 10 imaging exams were performed -- one patient was examined twice -- using a dose of 115 ± 13 MBq FDG based on the patient's body weight.
For the PET/CT studies, contrast-enhanced CT was performed as the diagnostic standard for all but two patients, who had a contraindication of renal impairment. Mean radiotracer uptake time was 62 ± 4 minutes, and mean total duration of the PET/CT examinations was 19 ± 8 minutes.
The PET/MRI scans were performed on a combined whole-body system with a 3-tesla MRI scanner. All exams were done without contrast, and PET and MRI were started simultaneously after a mean FDG uptake time of 115 ± 13 minutes. PET imaging lasted for four minutes per bed position. The mean total duration of the PET/MRI scans was 66 ± 20 minutes.
Hybrid comparisons
Two pairs of readers analyzed the PET/CT and PET/MRI results separately and independently. They found a total of 21 areas of focal FDG uptake in seven scans of six patients in both PET/CT and PET/MRI. The median lesion size was 14 ± 9 mm.
With PET/CT, seven suspicious lesions in four patients were identified as PET-negative, whereas PET/MRI found eight suspicious PET-negative lesions in five patients. The median lesion size was 10 ± 12 mm.
PET/CT and PET/MRI also differed in the number of malignant, benign, and uncertain lesions detected. The study's reference standard determined that 19 (65%) of 29 detected lesions were benign and 10 (34%) of 29 lesions were malignant.
| Lesion classification by modality | ||
| Status | PET/CT | PET/MRI |
| Benign | 9 | 13 |
| Uncertain | 12 | 7 |
| Malignant | 7 | 9 |
Of seven lesions that were interpreted differently by PET/CT and PET/MRI, six were PET-positive and had a clearer morphologic correlate in MRI compared to CT.
| Statistical measures by modality | ||
| Measure | PET/CT | PET/MRI |
| Sensitivity | 90% | 100% |
| Specificity | 47% | 68% |
| Accuracy | 62% | 79% |
Most importantly, five of 10 PET/MRI scans lead to potential changes in patient management, compared with PET/CT.
"This change in management affected the conduction of further imaging studies in four cases, which also means that an additional sedation could be saved in these cases using PET/MRI," the authors wrote.
This finding is of particular importance for this young pediatric population because anesthesia-related risks increase each time a child is sedated for subsequent imaging scans, Gatidis and colleagues noted.
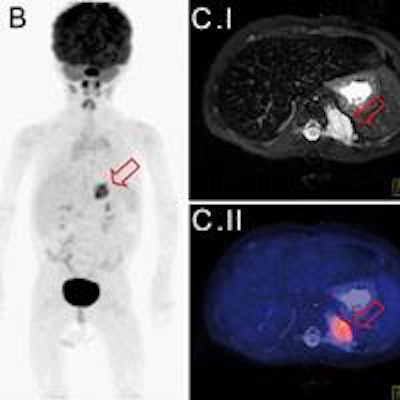
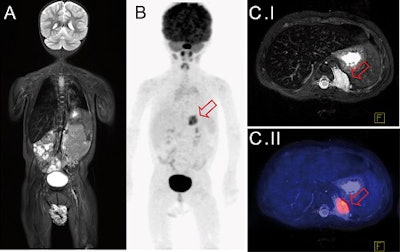 Whole-body FDG-PET/MRI exam of a 1-year-old girl with metastatic teratoma. Combined PET/MRI enables simultaneous acquisition of whole-body MRI (A) and PET (B) as well as local MRI (C.I). MRI shows a paravertebral metastasis (C.I, red arrow), which is metabolically active on FDG-PET (C.II, PET/MRI fusion image).
Whole-body FDG-PET/MRI exam of a 1-year-old girl with metastatic teratoma. Combined PET/MRI enables simultaneous acquisition of whole-body MRI (A) and PET (B) as well as local MRI (C.I). MRI shows a paravertebral metastasis (C.I, red arrow), which is metabolically active on FDG-PET (C.II, PET/MRI fusion image).The PET/CT results suggested an additional MRI scan for local staging and therapy planning for four patients, but the recommendation proved unnecessary except in one case.
"This additional examination [based on PET/CT] became unnecessary after PET/MRI, where local imaging was performed together with whole-body staging in one single examination," the authors wrote. "In one patient, the detection of a suspicious morphological MR correlate for focal tracer accumulation initiated close follow-up imaging and extended treatment."
While scan time for PET/MRI was significantly longer than for PET/CT, the PET/MRI scan duration was within the range of a comparable whole-body MRI scan for children.
"Compared with the time necessary for performing multiple different examinations (e.g., PET/CT and local MRI and a bone scan), PET/MRI may thus even help [decrease] total examination time as well as the number of examinations," they wrote.
The researchers noted several limitations of the study, including the small cohort. They added, however, that the comparison of PET/MRI and PET/CT on the same day allows for "substantiated conclusions, especially about technical feasibility and quantitative accuracy of PET/MRI."
FDG-PET/MRI is "technically feasible and at least equivalent to FDG-PET/CT for staging and tumor characterization of oncologic disorders in young children," the group concluded, adding that PET/MRI "has the potential of becoming the imaging reference standard in pediatric oncologic imaging for selected indications."