
Several presentations at the 2007 RSNA meeting in Chicago will explore ways to examine the rotator cuff with MRI. One education exhibit (LL-MK3292) will take a look at the utility of the abduction and external rotation (ABER) position in routine MR arthrography (MRA). A scientific paper (SST15-05) will verify the value of MRA for partial thickness rotator cuff tears, while another scientific poster will pit MR against ultrasound for detecting and measuring tears (LL-MK4129-B05).
Meanwhile, in a new American Journal of Roentgenology paper, Irish radiologists and orthopedists evaluated the correlation between MR findings and outcome after fluoroscopically guided subacromial bursography and steroid injection. The latter is a common way to nonoperatively treat rotator cuff impingement.
Of course, impingement must be identified before it can be managed, so a U.S.-based group tested out the ABER positions in an open-bore magnet for visualizing the mechanics of internal shoulder impingement.
Regular rotation
The ABER position is commonly used for clinical examination of the shoulder as well as for a closed-bore MR study. But in the latter, the ABER position is limited in terms of the ability to add load to the patient's arm, according to Dr. Garry Gold and colleagues at Stanford University Medical Center in Stanford, CA. Other study authors are from Massachusetts General Hospital in Boston and the University of Virginia in Charlottesville.
The group decided to test unloaded and loaded ABER positions in an open MR imaging unit in eight healthy male volunteers who had no history of shoulder pain. "The current results ... should enable clinicians to better understand which structures (in the shoulder girdle) are in contact during physical examination," the authors wrote (Radiology, September 2007, Vol. 242:3, pp. 815-821).
For this research, orthopedic surgeon Dr. Gordon Campbell examined the volunteers' right shoulders and determined that the apprehension sign, with the shoulder in the ABER position, was negative. The subjects were imaged in a 0.5-tesla scanner (Signa SP, GE Healthcare, Chalfont St. Giles, U.K.) in three different positions:
- Neutral with arm resting at side
- Unloaded ABER position
- Loaded ABER position with 1-kg load applied at the wrist
The MR protocol included 3D GRE sequences in the neutral arm in the coronal and transverse planes. Transverse images were acquired with the arm in the unloaded and loaded ABER positions. Finally, a 3D GRE sequence with repetition was used to facilitate segmentation.
Gold and co-author Dr. Christopher Beaulieu, Ph.D., read all the images, visually grading infraspinatus and suprasinatus tendon contact with the glenoid in neutral, unloaded, and loaded ABER positions. The highest score of 2 meant there was contact with deformation of the supraspinatus or infraspinatus.
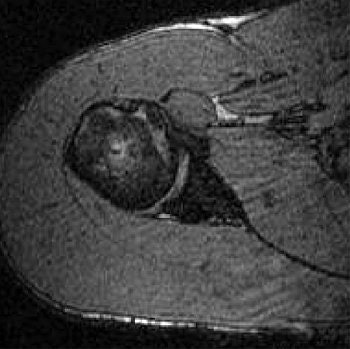 |
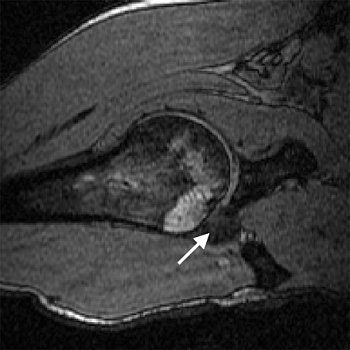
| Transverse 3D gradient-echo MR images (30/10) with volunteer in neutral position (above), unloaded ABER position at 90° external rotation (middle), and 111° external rotation (below). Note infraspinatus tendon (arrow) deformed between the greater tuberosity and posterosuperior glenoid in the loaded study. |
 |
 |
| Figure4a,b,c. Gold GE, Pappas GP, Blemker SS, et al. "Abduction and external rotation in shoulder impingement: an open MR study on healthy volunteers -- initial experiences." Radiology 2007; 244(3):815-822. |
Based on the image evaluation, contact was observed between the supraspinatus and the posterosuperior glenoid in the unloaded and loaded ABER positions in all eight volunteers. Again, in all eight subjects, contact was noted between the infraspinatus near the insertion and posterior glenoid in the loaded and unloaded positions. Four cases were deemed grade 2. Intraobserver agreement between the two radiologists on supraspinatus and infraspinatus tendon contact with the glenoid was excellent (k = 0.875).
The researchers also assessed minimum distances and noted changes in distance in the loaded ABER position. They found that the minimum distance between the supraspinatus insertion and the acromion dipped from 16.9 mm to 5.7 mm, while the infraspinatus to glenoid distance went from 38.4 mm to 3.6 mm. The supraspinatus to glenoid distance went from 35 mm to 6.6 mm. Finally, the distance between the greater tuberosity and glenoid decreased from 21.5 mm to 3.6 mm.
This last result suggested that "a larger portion of the greater tuberosity (including the supraspinatus and infraspinatus insertions) may be important in the minimum distance measurement," the authors stated. "The infraspinatus insertion, in particular, came to within 3.6 mm from the glenoid, on average."
The group came up with a couple of recommendations based on the results. First, a decrease in minimum distance may not translate directly to clinical impingement because contact between the rotator cuff and glenoid occurs even in asymptomatic individuals during the loaded ABER position. Also, the loaded position may be more specific for internal, rather than subacromial, impingement.
In addition, Gold told AuntMinnie.com that these relationships on loaded ABER position would be difficult to view on a conventional MR and are best seen with an open magnet.
Impingement
The nonoperative management strategies for rotator cuff impingement and subacromial bursitis include anti-inflammatory drugs and subacromial steroid injection. Dr. Niamh Hambly and colleagues recorded the clinical effect of image-guided subacromial steroid injection in patients with MRI-proven subacromial impingement syndrome. They also wanted to correlated outcome with patient age, duration of symptoms before injection, and preprocedural MRI results.
Hambly's group hails from Mater Misericordiae University, the Cappagh National Orthopaedic Hospital, and University College Dublin, all in Dublin.
Sixty-nine patients with clinical and MRI evidence of impingement made up the study population. Shoulder MRI was performed on a 1.5-tesla scanner (Avanto, Siemens Medical Solutions, Malvern, PA; or Intera, Philips Medical Systems, Andover, MA) with a dedicated coil. The MR protocol included coronal oblique T2-weighted images, coronal oblique STIR images, and axial gradient-echo images. Findings were graded on a five-point scale:
|
Grade 1: isolated subacromial bursitis |
For treatment, fluoroscopically guided subacromial bursography was performed and the injection consisted of 80 mg of methylprednisolone as well as 1-2 mL of 0.25% bupivacaine.
Of the 69 patients, the majority (40 or 58%) reported complete resolution of symptoms after six months of follow-up. Twelve (17%) people reported no symptom change, with four reporting that the symptoms were back to baseline six months later. Seventeen patients (25%) said they had partial symptom relief with a reduction in pain.
 |
| A 46-year-old woman with inflammatory changes in acromioclavicular joint with osteophyte formation, secondary impingement, and bursitis (grade 2). Symptom duration was four months, and patient reported complete resolution of symptoms after six months of follow-up. Subacromial bursogram shows inflammatory changes in acromioclavicular joint. |
The authors found that patients of all ages (mean age of 48.6) benefited from treatment. Of the 40 who reported complete resolution, 40% had duration of symptoms of less than three months. In terms of MRI grade, in those patients with partial resolution or no change, the MRI grade increased. They noted that the "mean duration of symptoms was significantly shorter among patients with complete resolution than those without" (American Journal of Roentgenology, November 2007, Vol. 189: 1179-1184).
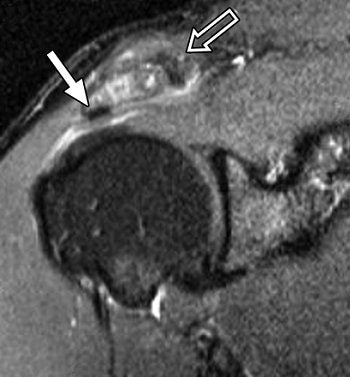 |
| Same patient as above. Symptom duration was four months, and patient reported complete resolution of symptoms after six months of follow-up. Coronal oblique STIR MR image (TR/TE, 2,000/20; inversion time, 160 msec; echo-train length, 8) shows changes in acromioclavicular joint (open arrow) with osteophyte formation (closed arrow). Hambly N, Fitzpatrick P, MacMahon P, and Eustace SW, "Rotator Cuff Impingement: Correlation Between Findings on MRI and Outcome After Fluoroscopically Guided Subacromial Bursography and Steroid Injection" (AJR 2007; 189:1179-1184). |
Overall, the authors found that better outcome was associated with shorter duration of symptoms, minor-grade MRI findings (1 and 2), and younger patient age. Given that 83% of the patients reported some form of relief after steroid injection, the authors concluded that the procedure has value for the short-term management of subacromial bursitis. A lack of response to treatment should prompt a search for an alternative cause, such as nerve root impingement, they suggested.
"In effect, MRI of the shoulder may be of benefit to patients ... because it allows confirmation of the diagnosis and allows the operator to predict which patients are more likely to respond to ... targeted steroid injection," the authors stated.
By Shalmali Pal
AuntMinnie.com staff writer
November 9, 2007
Related Reading
Fluoroscopically guided steroid injection effective in hip osteoarthritis, August 22, 2007
MRI keeps pace with rapidly evolving musculoskeletal systems of young athletes, May 20, 2007
US shows full spectrum of shoulder injuries, September 29, 2006
No slam dunk: Partial cuff tears defy MRI, US diagnosis, June 17, 2005
Copyright © 2007 AuntMinnie.com




















