
High-resolution short-tau inversion-recovery (STIR) MRI without contrast is feasible for the simultaneous evaluation of lower cranial nerves and the vessels in the posterior fossa, according to a study in the September issue of the American Journal of Roentgenology.
While additional research is needed, researchers from the Kyushu University in Fukuoka, Japan, say the MRI technique may be beneficial for imaging patients with neurovascular compression, which can cause severe pain and swelling in the face (trigeminal neuralgia), tongue, ear, nose, and tonsils (glossopharyngeal neuralgia).
Because STIR performs so well without contrast, patients with neurovascular compression can undergo MR imaging with no fear of an allergic reaction to the agent or potentially developing debilitating nephrogenic systemic fibrosis (NSF). Lead study author is Dr. Akio Hiwatashi from the department of clinical radiology and the Graduate School of Medical Sciences (AJR, Vol. 199:3, pp. 644-648).
No-contrast MRI
The posterior cranial fossa is part of the intracranial cavity and contains the brain stem and cerebellum. Prior to neurovascular decompression surgery, clinicians traditionally have used imaging techniques such as 3D T2-weighted MRI and 3D MR angiography (MRA), with or without contrast administration, to detect abnormalities.
"3D STIR images may reveal both cranial nerves and vessels simultaneously without the use of contrast," Hiwatashi and colleagues noted. "However, to our knowledge, there has been no study of visualization of these structures."
The retrospective study included 26 women and 21 men with a median age of 57 years, ranging from 35 to 86 years. There were 36 patients diagnosed with lung cancer and 11 cases of breast cancer.
All 47 subjects received MRI with a 3-tesla system (Achieva, Philips Healthcare) with an 8-channel head coil for the suspicion of brain metastasis. Images were obtained after administration of an MRI contrast agent (Magnevist, Bayer HealthCare Pharmaceuticals; Omniscan, GE Healthcare; or ProHance, Bracco Diagnostics) at a rate of 0.1 mmol/kg.
Participants were imaged with 3D STIR and turbo spin-echo T2-weighted MRI sequences, and with contrast-enhanced turbo field-echo MRA.
Two board-certified neuroradiologists reviewed and compared the images based on how well the MRI techniques were able to visualize the cranial nerves. Specifically, STIR images were graded on a four-point scale and compared with T2-weighted images. In addition, visualization of the arteries and veins via STIR were evaluated according to segments in each artery and compared with results with MRA.
The four-point image grading scale was used on the fifth through 12th cranial nerves, rating the results from no visualization (0), to poor results (1), moderate visualization (2), and good results (3).
Because of their close proximity in the cistern, the ninth through 11th nerves were graded as 0 for no visualization, 1 for poor visualization, 2 for excellent visualization and poor division into the pars nervosa and pars vascularis, and 3 for excellent visualization and sharp division into pars nervosa and pars vascularis.
After evaluating the various MRI techniques, Hiwatashi and colleagues concluded there were no significant differences between STIR and T2-weighted images in the visualization of the cranial nerves. The visualization of the fifth, seventh, and eighth cranial nerves also was deemed excellent with both imaging sequences.
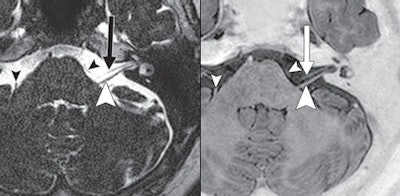 |
| A 70-year-old woman with lung cancer and no brain metastasis. The STIR MRI (right) shows seventh (arrow) and eighth (large arrowhead) cranial nerves and transverse pontine vein. T2-weighted MRI also shows seventh (arrow) and eighth (large arrowhead) nerves and transverse pontine vein (small arrowheads). Images courtesy of the American Journal of Roentgenology. |
While the researchers described the visualization of the sixth and lower cranial nerves as worse than that of the other nerves, they also concluded there was no statistically significant difference between the two techniques, as measured by the reader scores.
In their comparison, they found that STIR and T2-weighted MR images were almost identical, with all image ratings for the fifth, seventh, and eighth cranial nerves rated 3 (good results). On STIR images, 72 (77%) sixth cranial nerves were graded 3, while 20 (21%) cranial nerves were graded 2, and two (2%) cranial nerves were rated as 1. T2-weighted images achieved a 3 rating for 70 (74%) nerves, 20 (21%) cranial nerves were graded 2, and four (4%) cranial nerves received a 1.
Based on the ninth through 11th cranial nerves, STIR images were give a 3 on 46 (49%) nerve complexes, 46 (49%) nerves were assessed a 2, and two (2%) nerves were graded 1. T2-weighted images achieved a 3 on 50 (53%) nerve complexes, 37 (39%) nerves were give a 2 grade, and seven (7%) nerves were graded 1.
With STIR images, 12th cranial nerves were graded 3 in 11 (12%) cases and 71 (76%) were graded as 1. T2-weighted images received a 3 on four (4%) 12th cranial nerves, while 20 (21%) nerves were rated as 2, and 70 (75%) nerves were given a 1.
Based on the results, Hiwatashi and colleagues concluded that they were able to visualize both the nerves and the blood vessels of the posterior fossa on STIR MR images without using contrast material, and the visualization was similar to that of T2-weighted and contrast-enhanced MRA images.
"To the best of our knowledge, this report is the first of unenhanced imaging of small venous structures in the posterior fossa," they wrote. "Although further investigation is needed, our results suggest that use of STIR sequences may be best for evaluation of the anatomy of the cranial nerves, arteries, and veins that cause neurovascular compression."




















