As more studies weigh the risks and benefits of gadolinium-based contrast agents (GBCAs), German researchers have discovered that switching from a linear GBCA to a macrocyclic GBCA reduced the level of residual signal intensity in the brains of patients who underwent multiple enhanced MRI scans with both types of agents.
While the researchers declined to state that macrocyclic GBCAs were safer than linear agents, they recommended that the findings "be included in the risk-benefit evaluation when choosing the most appropriate GBCA for patients who need repeated follow-up examinations" (Investigative Radiology, November 2016, Vol. 51:11, pp. 683-690).
 Dr. Alexander Radbruch from the University of Heidelberg.
Dr. Alexander Radbruch from the University of Heidelberg."The most important advice is that patients should be informed that no clinical correlates of hyperintensities and gadolinium deposition are known yet," wrote lead author Dr. Alexander Radbruch, from the University of Heidelberg, in an email to AuntMinnie.com. "Common sense dictates that we should minimize the gadolinium deposition in the patients. Therefore we recommend the inclusion of the 'gadolinium deposition risk' in the risk-benefit evaluation prior to the injection of a GBCA."
The GBCA debate
Several retrospective studies over the past several years have found that patients who received repeated administrations of gadolinium contrast had increased signal intensity in areas of their brains on unenhanced T1-weighted MR images, long after they underwent MRI scans. While the locations of the signal intensities have varied, the dentate nucleus has received much attention, in part because it is key to the body's central nervous system.
In fact, Radbruch et al published a 2015 study that found greater signal intensity in the dentate nucleus and globus pallidus among patients who received the linear GBCA gadopentetate dimeglumine. There was no such escalation in patients who had received the macrocyclic GBCA gadoterate meglumine, despite the fact that a substantially larger dose of contrast was used in the latter group.
"Since we changed our standard GBCA in our institution from linear to macrocyclic GBCAs in 2009, we could assess signal intensity changes in the dentate nucleus in patients who first received serial injections of linear and subsequent serial injections of macrocyclic GBCAs," Radbruch said.
A number of studies have found that the best way to measure gadolinium deposition in the dentate nucleus is by calculating a ratio that compares the signal from the dentate nucleus to that of the pons; if there is an increase in the ratio it suggests higher levels of gadolinium deposition in neural tissue. In addition, most studies found no increase in the dentate nucleus-pons signal ratio when patients were treated with macrocyclic GBCAs.
However, as the authors noted, "the potential difference between macrocyclic and linear GBCAs has never been assessed in individuals who received subsequent applications of both contrast agents."
GBCA comparisons
Radbruch and colleagues retrospectively reviewed patients who had multiple MRI scans between June 2008 and February 2009 during the institution's transition from a linear GBCA to two different macrocyclic GBCAs.
Under the study inclusion criteria, 36 patients qualified by receiving five or more administrations of the linear GBCA gadopentetate dimeglumine (Magnevist, Bayer HealthCare) and then the macrocyclic agent GBCA gadobutrol (Gadavist, Bayer) (GBCA-1). Among the 36 patients, 12 also received five or more additional administrations of the second macrocyclic GBCA, gadoterate meglumine (Dotarem, Guerbet) (GBCA-2).
MRI scans with the linear GBCA and macrocyclic GBCA-1 were performed on a 3-tesla scanner (Trio and/or Verio, Siemens Healthineers) or a 1.5-tesla scanner (Symphony, Siemens). MRI exams with the macrocyclic GBCA-2 were performed on a 3-tesla scanner (Trio and/or Verio, Siemens).
To create the signal intensity ratios, the researchers drew regions of interest (ROIs) on the central pons from unenhanced T1-weighted MR images and around the right and left dentate nuclei using T2-weighted images for guidance. From those ROIs, average signal intensities of the right and left dentate nuclei were calculated and divided by the mean signal intensity of the central pons to create the dentate nucleus-to-pons ratios for all three GBCAs.
Ratio results
Radbruch and colleagues found a statistically significant increase in the dentate nucleus-pons signal ratio on unenhanced T1-weighted MR images after serial administrations of the linear GBCA; however, the ratio declined in the same patients who proceeded to receive subsequent injections of the two macrocyclic GBCAs.
| Mean dentate nucleus-pons signal ratio | |||
| Linear GBCA | Macrocyclic GBCA-1 | Macrocyclic GBCA-2 | |
| Increase or decline in dentate nucleus-pons signal ratio | 0.0448 ± 0.0345 | -0.0178 ± 0.0459 | -0.0250 ± 0.0284 |
| p-value | < 0.001 | 0.026 | 0.011 |
"Interestingly, we also found evidence for a signal intensity decrease of pre-existing hyperintensities when linear GBCAs were changed to macrocyclic GBCAs," Radbruch said. "It is important to note that this decrease was rather small and the evidence provided in the study is limited."
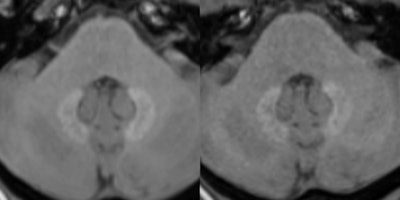 Unenhanced T1-weighted MR images at 3 tesla depict a patient with pre-existing hyperintensities in the dentate nucleus. The left image displays the cerebellum prior and the right image after five serial injections of the macrocyclic GBCA Gadavist. A subtle decrease of the pre-existing hyperintensities can be noted. Images are courtesy of Dr. Alexander Radbruch.
Unenhanced T1-weighted MR images at 3 tesla depict a patient with pre-existing hyperintensities in the dentate nucleus. The left image displays the cerebellum prior and the right image after five serial injections of the macrocyclic GBCA Gadavist. A subtle decrease of the pre-existing hyperintensities can be noted. Images are courtesy of Dr. Alexander Radbruch.The researchers speculated on four reasons for the decrease in signal intensity of pre-existing hyperintensities. Radbruch said the potential signal intensity decrease is most likely not connected with the injection of macrocyclic GBCAs, but it might be explained by a washout of the gadolinium, precipitation of the gadolinium over time, or a combination of both mechanisms. In addition, some gadolinium may have been eliminated through excess ligands, or the decrease may be due to a signal increase in the pons, which could have affected the ratios.
Clinical relevance
"On a practical clinical level, our findings might be relevant for patients who need regular follow-up examinations and who are concerned because of pre-existing hyperintensities caused by previous injections of linear GBCAs," Radbruch said. "Our data provides evidence that pre-existing hyperintensities in the dentate nucleus at least do not further increase if linear GBCAs are changed to macrocyclics."
Naturally, Radbruch and colleagues recommended additional human and animal studies to replicate and validate their results, along with the inclusion of control subjects.
"In my opinion, we still need a lot of education and information of the radiological community in this field. It is especially important for the information of concerned patients," Radbruch noted in his email. "Even though we do not know if the hyperintensities/gadolinium depositions have any clinical meaning, common sense dictates that we should avoid them, if possible."



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)




.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)