The combination of ultrasound- and MRI-guided biopsy yields the best chance of detecting prostate cancer, as each method can find malignant lesions missed by the other, researchers from the University of California, Los Angeles (UCLA) reported in a study published online June 12 in JAMA Surgery.
In the three-year Prospective Assessment of Image Registration in the Diagnosis of Prostate Cancer (PAIREDCAP) study, the researchers found that using ultrasound and MRI in tandem can identify up to one-third more cancers than standard techniques.
"Our research suggests that the different biopsy methods identify different tumors," said senior author Dr. Leonard Marks, from UCLA's department of urology, in a statement. "To maximize our ability to identify prostate cancer, we need to take advantage of all the information we can. Our cancer detection rate, while using different methods in tandem, surpasses that from using either method alone."
While the clinical value of MRI-guided prostate biopsy has been proved in previous large prospective studies, some debate remains over the optimum approach with the modality. Clinicians have debated whether biopsy should focus on areas with lesions only visible on MRI or if ultrasound-guided systematic biopsy -- in which 12 biopsy cores are acquired of multiple areas of the prostate -- is sufficient.
"Answers to these questions are vital because of the importance of diagnosing prostate cancer early vis-a-vis cost-effectiveness issues," the authors wrote.
The prospective study included 300 men who were undergoing prostate biopsy for the first time: 248 consecutive subjects (mean age, 65.5 ± 7.7 years) had MRI-visible lesions, while the control population consisted of 52 men (mean age, 63.6 ± 5.9 years) with no visible lesions on MRI. Each biopsy was preceded by a 3-tesla multiparametric MRI scan (Magnetom Trio, Siemens Healthineers) with an abdominal coil within 60 days of the procedure.
The study protocol used three biopsy techniques:
- Systematic biopsy, performed with a standard handheld transrectal ultrasound-guided technique in which 12 cores were acquired, with the operator blinded to the MRI results
- Targeted cognitive fusion, in which a radiologist used MR images on a screen next to the patient to guide the urologic biopsy operator to aim an ultrasound-guided biopsy at the area of the prostate corresponding to where the lesion was seen on MRI; three biopsy cores were obtained cognitively from the index region of interest (ROI)
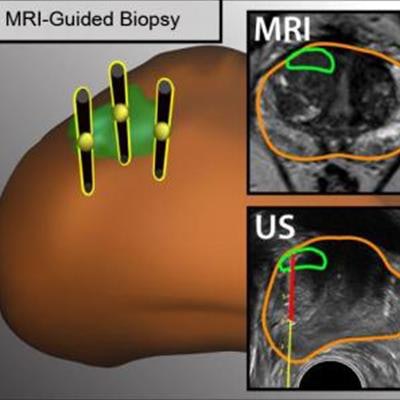
- Software fusion, in which researchers fused MRI and 3D ultrasound images using commercially available software (Artemis, Eigen), and an operator performed three targeted biopsies on the coregistered images
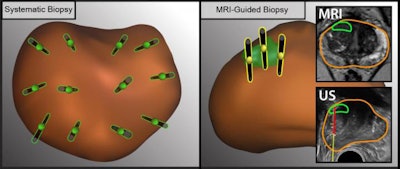 The illustration shows the difference between ultrasound- and MRI-guided methods to obtain tissue samples (black needles) from different regions in the prostate (brown oval object). MRI (right) allows doctors to detect lesions (green oval object) and take tissue samples from specific lesions. Images courtesy of UCLA Health.
The illustration shows the difference between ultrasound- and MRI-guided methods to obtain tissue samples (black needles) from different regions in the prostate (brown oval object). MRI (right) allows doctors to detect lesions (green oval object) and take tissue samples from specific lesions. Images courtesy of UCLA Health.The combination of methods produced the highest results, the researchers found.
| Cancer detection rate of prostate biopsy methods | |
| Biopsy method | Cancer detection rate |
| Combination of systematic, cognitive, and software fusion biopsy | 70.2% |
| Cognitive fusion or software fusion | 62.1% |
| Cognitive targeting | 46.8% |
The cancer detection rate of 70% is considerably higher than the cancer detection rate of conventional biopsy in previous studies, likely reflecting the outcomes of the MRI screening, the researchers noted. "These data thus serve to confirm the value of MRI for providing risk assessment when considering biopsy," they wrote.
Indeed, the researchers found that if only a single biopsy method was used, from 11.5% to 33.3% of cancers would have been missed, based on patient population.
Interestingly, among the 52 healthy controls, traditional ultrasound found prostate cancer in eight men (15%). This means that MRI does not identify all tumors, thus heightening the need to also incorporate traditional ultrasound-guided systematic biopsy as well, according to the researchers.