MR images have revealed decreased cortical thickness in people on antipsychotic drugs compared with those on placebo. But in both cases, their relapse back into psychosis may be due more to structural brain change than a lack of medication, according to a study published February 26 in JAMA Psychiatry.
The results are particularly noteworthy because antipsychotic drugs are given to young and old patients for a variety of conditions -- and the risks include increased possibility of sudden, unexpected death. Such potential outcomes could change the scale when weighing whether to put a patient on medication.
"Our findings could support a reconsideration of the risks and benefits of antipsychotics and support differential effects on brain structure in those who stay well receiving placebo versus those who relapse," wrote the authors, led by Dr. Aristotle Voineskos, PhD, from the Centre for Addiction and Mental Health in Toronto, Canada.
Antipsychotic drugs have been prescribed primarily for people with schizophrenia. But their use has expanded to pediatric patients to treat autism, to adults, and to geriatric patients with mood disorders. The danger is that the medications are associated with a greater risk of mortality, especially for children and elderly individuals.
"Despite their risk, antipsychotics remain the foundation of treatment for schizophrenia, in part because it is believed that antipsychotics protect against the harmful effects of untreated psychosis on the brain," the authors noted. "However, data suggest that both older and newer antipsychotic medications may be associated with changes in gray-matter and white-matter structure."
To determine what effect, if any, antipsychotic drugs have on brain structure and patient outcomes, Voineskos and colleagues proposed a placebo-controlled trial in which they compared patients who received olanzapine to treat schizophrenia and depression and subjects who received the sham treatment.
The researchers recruited participants (range, 18-85 years) from the multicenter Study of the Pharmacotherapy of Psychotic Depression II (STOP-PD II) who were diagnosed with nonbipolar major depressive disorder. Subjects received olanzapine and sertraline for 12 to 20 weeks, which included eight weeks of remission from psychosis and depression. They then were randomized into one group (38 people; mean age, 54.4 years) that continued to receive olanzapine and a second group (34 people; mean age, 54.4 years) that received a placebo for 36 weeks.
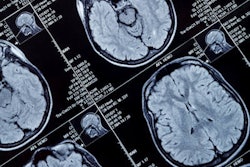
The 72 participants underwent 3-tesla MRI scans at the start of the study and at the end of the 36-week treatment regimen or when and if they relapsed back into psychosis. The protocol included diffusion-tensor MR imaging (DTI-MRI) to evaluate white matter microstructure, while high-resolution T1-weighted imaging was used to evaluate gray matter structure via cortical thickness, surface area, and subcortical volume.
MRI results revealed a significant decrease in cortical thickness in both the left and right hemispheres of people who were treated with olanzapine and did not relapse, compared with subjects in the placebo group. In addition, people who received the placebo and relapsed showed decreases in cortical thickness, compared with others in the placebo group who stayed in remission.
This result would suggest that cortical thickness is a more influential contributor to relapse into psychosis than an antipsychotic drug.
"While our data show that antipsychotics may cause adverse changes to brain structure, they also demonstrate that illness relapse may cause similar effects," the researchers concluded. "When psychosis is present, the life-threatening effects of untreated illness outweigh any adverse effects on brain structure in clinical decision-making."