Brain MRI scans showed no significant differences in Alzheimer's disease biomarkers among patients on intensive blood pressure therapy compared with patients on standard therapy in a study published online March 8 in JAMA Neurology.
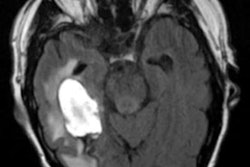
Researchers led by radiologist Dr. Ilya Nasrallah, PhD, of the University of Pennsylvania studied the MRI scans of 454 hypertensive patients who were 50 years or older and completed a brain MRI at baseline and then at four-year follow-up in July 2016. Among the two patient groups, they compared hippocampal volume, measures of Alzheimer's disease regional atrophy, posterior cingulate cerebral blood flow, and mean fractional anisotropy (FA) in the cingulum bundle.
"There is no consistent or clinically meaningful difference in magnetic resonance imaging biomarkers of Alzheimer's disease between intensive and standard blood pressure treatment," Nasrallah and colleagues wrote.
Vascular disease is a common comorbidity and may play a factor in initiating or accelerating hippocampal atrophy and mild cognitive impairment (MCI), characteristic biomarkers of Alzheimer's disease. Some studies have found that treating hypertension may reduce the incidence of Alzheimer's disease, but no clear mechanism has been identified.
This study's authors hypothesized that intensive treatment would be associated with less atrophy, as seen on MRI scans by hippocampal volume and Alzheimer's disease regional cortical thickness. They also looked for an increase in perfusion in the posterior cingulate gyrus and a smaller decrease in fractional anisotropy in the cingulum bundle.
A total of 673 participants completed baseline MRI scans with a measurement of total brain volume, and 454 of this group completed follow-up MRI studies. At baseline, the mean age of participants was 67.3 years; 40.3% were female and 32.4% were Black. Mean blood pressure was 138.1/77.9 mmHg.
Intensive blood pressure treatment was associated with a small but statistically significant greater decrease in hippocampal volume. In the intensive treatment group, mean hippocampal volume decreased from 7.45 cm3 to 7.39 cm3, compared with a decrease from 7.48 cm3 to 7.46 cm3 in the standard treatment group.
But there was no evidence of a treatment group difference for any of the other markers of neurodegeneration that can be signs of a progression to Alzheimer's disease, the researchers wrote.
The present study was a secondary analysis of the U.S. National Institutes of Health-funded Systolic Blood Pressure Intervention Trial - Memory and Cognition in Decreased Hypertension (SPRINT MIND), which help guide the development of new clinical guidelines on high blood pressure from the American Heart Association and American College of Cardiology in 2017. The final MRI follow-up date in this study was July 1, 2016, while analysis of data began in September 2019 and ended in November 2020.
Early changes in Alzheimer's disease are challenging to detect even with biomarkers that strongly correlate with disease severity, especially in populations consisting of largely cognitively normal individuals. That was the case here, as patients with dementia were excluded from the trial, the authors wrote. There were several additional limitations, including that early Alzheimer's disease-related neurodegeneration also develops slowly, so that the four-year follow-up may have been too short.
The authors made clear that these MRI findings do not directly identify a specific pathologic mechanism for the link between intensive blood pressure treatment and brain structure or the development of cognitive impairment.
In an accompanying editorial, Susan Landau, PhD, and Theresa Harrison, PhD, both of the University of California, Berkeley, discussed the research challenges involved in finding new disease-modifying treatments for Alzheimer's disease, as a number of major recent clinical trials of drug therapies have resulted in negative or ambivalent findings.
Two key strategies are emerging: initiating interventions earlier in the course of disease in individuals who are at risk but unimpaired and identifying targets beyond abnormal amyloid and tau proteins. Longitudinal imaging data in large, rigorous, multisite clinical trials like SPRINT MIND are valuable because they may help establish a causal link between hypertension and the brain, whereas epidemiological data cannot.
Identification of the underlying Alzheimer's disease pathophysiology that drives the incidence of decreased MCI would be "ground-breaking" in that it would establish a definitive link between hypertension control and reduced risk of the disease, Landau and Harrison wrote.