MRI isn't yet ready to replace prostate-specific antigen (PSA) testing as a first-line screening exam for prostate cancer, researchers have reported.
A team led by Roman Gulati of Fred Hutchinson Cancer Center in Seattle found that "despite the potential attractiveness of first-line imaging-based [prostate cancer] screening, [a] microsimulation model showed that first-line [biparametric MRI]-based screening substantially increased rates of false-positive test results, prostate biopsy, and overdiagnosis without proportionately substantial reductions in prostate cancer mortality compared with first-line PSA testing with reflex [multiparametric MRI]." The study findings were published June 3 in Annals of Internal Medicine.
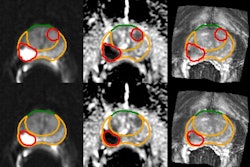
First-line prostate cancer screening is currently performed with PSA testing, and in men with elevated PSA levels, may be followed by multiparametric MRI (mpMRI). In recent years, first-line biparametric MRI (bpMRI) screening has been proposed as an alternative to mpMRI; bpMRI uses T2-weighted images with diffusion-weighted imaging [DWI], while mpMRI adds dynamic contrast-enhanced [DCE] imaging -- with or without spectroscopy, the authors explained.
The draw of using MRI to diagnose prostate cancer is that it could streamline patient care, according to an editorial that accompanied the study.
"Replacing PSA testing with MRI would reduce the need for multiple consultations, thereby possibly improving efficiency and patient satisfaction," wrote a team led by Daniel Joyce, MD, of Vanderbilt University Medical Center in Nashville, TN. "Biparametric MRI (bpMRI), which omits the contrast-enhanced phases and thereby decreases cost and study duration, has been shown to be equivalent to multiparametric MRI in cancer detection and may further increase the value of MRI use in prostate cancer screening."
Gulati and colleagues compared both clinical effectiveness and cost-effectiveness of bpMRI versus PSA-based for prostate cancer screening via a microsimulation model based on data from the Surveillance, Epidemiology, and End Results (SEER) database and randomized trials, culling information for 1,000 men aged 55 years with no prior prostate cancer screening or diagnosis.
The proposed intervention was biennial screening from 55 to 69 years using first-line PSA testing (test-positive threshold: 4 mg/L) -- with or without second-line mpMRI -- or first-line bpMRI (test-positive threshold: Prostate Imaging Reporting and Data System [PI-RADS] 3 to 5 or 4 to 5), followed by biopsy-guided MRI or MRI plus transrectal ultrasonography. The investigators tracked the types of screening tests, any biopsies, diagnoses, overdiagnoses, treatments, prostate cancer deaths, quality-adjusted and unadjusted life-years saved, and costs.
Gulati's group found the following:
| Comparison of first-line PSA testing to first-line bpMRI for prostate cancer screening in 1,000 men | ||
|---|---|---|
| Measure |
First-line PSA testing |
First-line bpMRI |
| Deaths prevented |
3 |
2 |
| Additional life years |
30 |
10 |
| Number of biopsies |
1,506 |
4,174 |
| Number of overdiagnoses |
38 |
124 |
It also found that using conventional cost-effectiveness thresholds, first-line PSA testing with mpMRI followed by either biopsy approach for men with PI-RADS 4 to 5 results demonstrated the greatest net monetary benefits.
"First-line PSA testing remained more cost-effective even if bpMRI was free, all men with low-risk [prostate cancer] underwent surveillance, or screening was quadrennial," the group wrote.
The study underscores a need for more research, Joyce and colleagues noted in their editorial.
"[This] cost-effectiveness analysis of a bpMRI-first prostate cancer screening approach highlights the need for a more robust understanding of the true comparative diagnostic accuracy of bpMRI compared with PSA testing followed by standard template biopsy, the financial toxicity associated with modern prostate cancer screening practices, and how to select the best patients for prostate biopsy through incorporation of biomarkers, imaging, and patient risk factors," they wrote. "While we await such evidence, rigorous cost-effectiveness analyses can and should be considered in guideline recommendations to encourage physicians to pursue the highest-value management strategy for their patients."
The complete study can be found here.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











