The Dutch example of breast cancer screening works, and mammography screening is a clear way of detecting cancer early, along with increased breast cancer awareness, according to the authors of a new study published in BMJ.
Women have a greater chance of five-year survival if breast cancer is detected early while tumors are small, fewer in number, and early-stage, noted the authors from Erasmus University Medical Center in Rotterdam. Although these factors have been thought to influence strongly a patient's prospects, it has been unclear to what extent, particularly when factoring in patient age, tumor behavior, and the wide range of modern therapies offered.
Their study involved 173,797 female patients with primary breast cancer from two time frames: 1999 to 2005 (80,228 patients) and 2006 to 2012 (93,569 patients), with data taken nationwide from the Netherlands' Cancer Registry. Date, age at breast cancer diagnosis, tumor characteristics, and treatments were taken into account (BMJ, October 6, 2015).
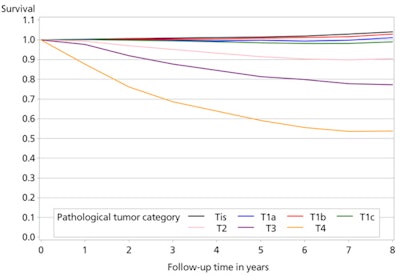 This graph gives the relative survival (compared with survival of women of the same ages in the Dutch population without breast cancer) of the most recent cohort. The lines stand for different tumor stages. Relative survival for all tumors up to 1 cm was 100%, thereafter survival decreases with increasing size. Tis = ductal carcinoma in situ, a premalignant lesion; T1a cancer 1-5 mm; T1b 5-10 mm; T1c 10-20 mm; T2 20-50 mm (2-5 cm); T3 > 5 cm; T4 cancer growing into the skin or the musculus pectoralis. All figures courtesy of Dr. Madeleine Tilanus-Linthorst, PhD.
This graph gives the relative survival (compared with survival of women of the same ages in the Dutch population without breast cancer) of the most recent cohort. The lines stand for different tumor stages. Relative survival for all tumors up to 1 cm was 100%, thereafter survival decreases with increasing size. Tis = ductal carcinoma in situ, a premalignant lesion; T1a cancer 1-5 mm; T1b 5-10 mm; T1c 10-20 mm; T2 20-50 mm (2-5 cm); T3 > 5 cm; T4 cancer growing into the skin or the musculus pectoralis. All figures courtesy of Dr. Madeleine Tilanus-Linthorst, PhD.Overall breast cancer survival improved in all tumor sizes and stages, and traditional prognostic factors such as stage and size at diagnosis are still crucial to patients' chances of survival, irrespective of age and tumor biology.
Compared with tumors diagnosed in 1999 to 2005, tumors diagnosed in 2006 to 2012 were smaller (65% or 60,570 patients with tumors smaller than 20 mm versus 60% or 48,031 patients in the earlier group), more often lymph-node-negative (68% or 63,544/93,569 versus 65% or 52,238/80,228) and more often low-grade (grade 1 invasive cancer 21% or 17,334/93,569 versus 16% or 11,939/80,228).
Relative survival rates, which compare breast cancer patients with Dutch women of the same age without the disease, and overall survival rates were higher in the 2006 to 2012 cohort for all tumor and nodal stages, and they improved the most in women 75 years of age and older. Relative survival of patients improved from 91% to 96% at five-year follow-up.
The findings are summarized in the table below.
| Diagnosis characteristics in Dutch screening program | ||
| Diagnosis characteristics | 1999 to 2005 | 2006 to 2012 |
| Percent of tumors 20 mm and smaller | 60% | 65% |
| Percent of lymph-node-negative tumors | 65% | 68% |
| Percent of low-grade invasive cancer | 16% | 21% |
| Relative survival rates | 91% | 96% |
Clear and positive messages
"The study provides several clear and positive messages," corresponding author Dr. Madeleine Tilanus-Linthorst, from the department of surgery at Erasmus, told AuntMinnieEurope.com. "First, survival for breast cancer patients has improved. Also in the recent group, increasing size was correlated with lower survival in tumors above 1 cm."
However, in tumors of up to 1 cm in size, relative survival was 100%, and more patients (65%) had tumors detected early (< 2 cm) in the recent cohort versus 60% in the older, she continued, adding that relative survival in the recent cohort for patients with tumors between 1 cm and 2 cm was at 98%.
"Survival has improved for every tumor stage and size, which is comforting," she noted. "Even patients diagnosed later with large tumors of 5 cm and above experienced an improvement in outcome. In the earlier group, such patients had a 70% five-year relative survival, while in the later cohort this increased to 81%."
 Positive information about patients' prospects can be both morale-boosting and informative, Tilanus-Linthorst said.
Positive information about patients' prospects can be both morale-boosting and informative, Tilanus-Linthorst said.The researchers also wanted to know what effect different treatments had on survival.
Patients from the 2006 to 2012 cohort more often had breast-conserving treatment, 54% versus 48%. In this later cohort, there was also more uptake of systemic therapies (hormonal, chemotherapy, or antiepidermal growth factor) to prevent metastasis, with 53% of patients in the older cohort receiving systemic therapy and 60% receiving it in the more recent cohort. Uptake of hormonal therapy in this recent patient cohort was 49% versus 39%, chemotherapy uptake was 37% versus 30%, and targeted therapy uptake was 8% versus 1%.
The study revealed that surgery was crucial; breast-conserving treatment seemed slightly more favorable than mastectomy (hazard ratio [HR] 0.87, p < 0.001), but comorbidity may have had some influence on this result. Contralateral cancer had no impact on survival.
Hormone and targeted drug therapies were also clearly beneficial, corrected for stage age and tumor biology. The benefit of chemotherapy (HR 0.86, p < 0.001) was smaller than hormone therapy (HR 0.64, p < 0.001) and targeted drug therapy (HR 0.58, p < 0.001).
"The impact of systemic therapy is clear. Size and stage still make a huge difference. Therefore, screening and breast cancer awareness are worth it," Tilanus-Linthorst said.
She believes it would be speculative to say for certain why there was earlier detection in the recent cohort, as evidenced by smaller tumors and fewer axillary nodes, but suggests it may have been partly because screening was more effective in the second time frame.
"In the Netherlands, screening changed to digital mammography in 2006, which may have helped earlier detection. Furthermore, women with the BRCA1 and BRCA2 genes at high risk are screened with MRI and mammography. MRI sensitivity increased in and after 2006, during which time the results of MRI and mammography also improved," she noted.
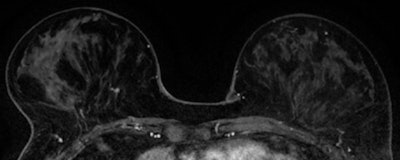 MR images of early detected invasive ductal carcinoma (grade II, 5 mm, SN 0/2).
MR images of early detected invasive ductal carcinoma (grade II, 5 mm, SN 0/2).The research team hopes that both patients and doctors, as well as the wider public, will read the results of the study, because it provides positive information about patients' prospects, which are both morale-boosting and informative.
"Stakeholders in therapy decisions will have a clear means to weigh up the different options in terms of their benefits. This is particularly important for women with comorbidities such as heart disease," Tilanus-Linthorst said.
With this in mind, the authors intend to disseminate the information from the study as widely as possible, through the medical media and patient groups. The general media have also shown interest in the data, particularly in light of the ongoing polemic on screening, driven by reports of high false-positive figures particularly across U.S. centers.