Radiologists who double read automated breast ultrasound scans (ABUS) on their own or in combination with digital breast tomosynthesis (DBT) had higher cancer detection rates -- but their recall rates were also higher, according to a recent study in the Journal of Breast Imaging.
As density reporting laws increase, more women are undergoing ultrasound as a screening tool. The authors wondered whether ABUS might serve as a natural complement to DBT or even stand on its own as a screening modality for women with dense breasts.
"To our knowledge, this is the only prospective study that includes simultaneous assessments of DBT and ABUS whether as supplementary and/or individual modalities with and without double reading," wrote the authors, led by Dr. Denise Chough from the University of Pittsburgh School of Medicine (J Breast Imaging, February 27, 2020).
Chough and colleagues recruited women ages 40 to 75 who visited one of two mammography centers in Pittsburgh for their routine screening between August 2015 and September 2018. All the women in the study were known to have heterogeneously dense or extremely dense breast tissue.
Technologists performed two-view DBT and ABUS imaging on all participants, often during the same visit. Then, two radiologists with at least 13 years of experience independently read the scans.
The primary radiologist specifically focused on DBT results, followed by DBT plus ABUS. The secondary radiologist focused on ABUS, followed by ABUS plus DBT. If the readers disagreed on the findings, the primary radiologist got the final say.
The primary radiologist recalled 160 women based on the combined DBT and ABUS findings, and seven of these women were diagnosed with cancer. However, the primary radiologist also missed one invasive ductal carcinoma that presented as shadowing.
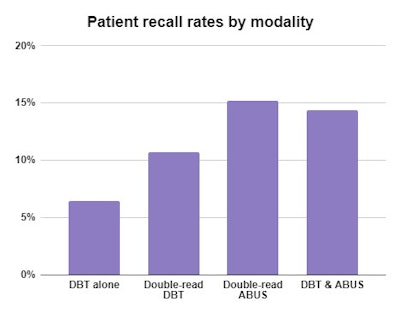
When the authors included the readings of the secondary radiologist as well, the double-read ABUS and DBT scans identified all known cancer cases in the cohort. But the recall rate also increased by almost 8 percentage points compared with the single-read DBT results.
"Our results indicate that although the use of ABUS could lead to detecting additional cancers missed by DBT, this practice is associated with a significant increase in recall rate, both in single, as well as double-reading settings," the authors wrote.
For double-read ABUS scans, 15% of women were recalled, and 7 women were diagnosed with cancer. However, the recall rates were drastically lower in the later years of the study, which the authors attributed to an increase in experience with ABUS and better availability of prior images.
The recall rate of double-read DBT scans was much lower than for ABUS -- 11% versus 15%. But double reading DBT only identified six cancer cases, all of which the primary radiologist had already independently identified.
"Interestingly, while the double reading of ABUS yielded an additional cancer detection, the double reading of DBT alone did not, perhaps reflecting our radiologists' greater experience with DBT," the authors wrote.
In addition to the radiologists' differing experience levels with ABUS and DBT, the study took place at a single institution, which could have impacted the results. Nevertheless, the findings suggest ABUS could be a supplemental screening method to DBT or even its own screening modality. However, the authors cautioned that larger, future studies will be needed to confirm the results.
"Indeed, in our study, the double reading of ABUS led to essentially the same recall rates and number of detected cancers as ABUS-supplemented DBT interpretations," the authors wrote. "Combined with the relative inexperience of radiologists with ABUS, this may indicate possible improvement of standalone ABUS performance in the future."