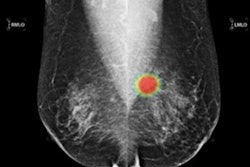
Swedish researchers found that artificial intelligence (AI)-based computer-aided detection software cut radiologists' screening mammogram workload by more than half. It also could catch more interval and future screening-detected cancers, according to a study published online August 24 in the Lancet: Digital Health.
After performing a retrospective simulation study involving screening mammograms from over 7,000 women, a team of Swedish researchers led by Dr. Karin Dembrower of the Karolinska Institute in Stockholm found that risk prediction scores from a commercial AI software application could have obviated the need for radiologists to review over 60% of these exams -- without missing any cancers.
What's more, an enhanced screening strategy that includes providing breast MRI for women with the highest AI scores could detect up to 27% of subsequent interval cancers and up to 35% of cancers found in the next round of screening, according to the group.
"AI-based scoring can be used to reallocate radiologist time from clearly negative mammograms toward cases where cancer might go undetected," the authors wrote. "AI has the potential to promote early detection and thereby increase overall survival for breast cancer patients."
The researchers had hypothesized that a substantial proportion of the population with the lowest AI risk scores on screening mammograms could be safely ruled out without missing any cancers that would have been detected by a radiologist. In addition, they hypothesized that women with the highest AI risk scores would have a high proportion of interval cancers that would have potentially been identifiable on MRI or another imaging modality.
Dembrower and colleagues tested those hypotheses by retrospectively applying commercial AI software (Lunit) to a study sample of 7,364 women (6,817 healthy controls and 547 women with a cancer diagnosis) ages 40 to 74 who had received mammograms between February 10, 2009, and December 10, 2015, at their institution. All mammograms were acquired on full-field digital mammography systems from Hologic.
Next, the researchers assessed the simulated use of AI in two different scenarios:
- Relying on algorithm prediction scores to triage cases as normal and therefore not requiring radiologist assessment
- Using algorithm prediction scores to recommend supplemental imaging (e.g. MRI) in women whose mammograms had high AI risk scores but who were interpreted as normal after double reading
| Proportion of missed screening-detected cancers if mammograms with low AI scores weren't read by radiologists | |||
| Low 80% of AI scores | Low 70% of AI scores | Low 60% of AI scores | |
| Missed cancers | 2.6% | 0.3% | 0% |
They also concluded that more interval and future screening-detected cancers could be found by using the highest AI risk scores to channel women into an expanded assessment protocol that included breast MRI.
| Potential additional cancer detection rate by percentage of women with high AI scores but negative mammograms | ||
| Top 1% of AI scores | Top 5% of AI scores | |
| Subsequent interval cancer detections | 24 of 200 (12%) | 53 of 200 (27%) |
| Cancers detected in the next round of screening | 48 of 347 (14%) | 121 of 347 (35%) |
"After AI algorithm scoring of mammograms, the lowest 60% could be triaged to a no radiologist work stream without missing any cancer that would otherwise have been screen detected," the authors wrote. "Then, after negative radiologist assessment of the remaining mammograms, the highest AI scores could be used to identify mammograms for an enhanced assessment work stream with a substantial enrichment of false-negative assessments."
The authors noted that retrospective trials in other settings and a prospective trial would be needed to validate their results.