Although digital breast tomosynthesis (DBT) can improve breast cancer detection, false-negative results still occur. Two studies presented at the American Roentgen Ray Society (ARRS) annual meeting in Honolulu characterized these missed cancers.
After retrospectively analyzing cases of false-negative findings on DBT, groups led separately by Dr. Wenhui Zhou from Stanford University Medical Center and Dr. Manisha Bahl from Harvard Medical School found that these misses tended to have certain characteristics and notably often involved dense breasts.
"Increased vigilance to areas of high density in women with dense breasts might help to avoid delayed diagnosis in this patient population," Zhou said.
False-negative characteristics
Zhou and colleagues' eight-year study sought to identify clinical and imaging determinants of false-negative results in DBT breast cancer screening. The team retrospectively reviewed 69,594 screening DBT studies performed between March 2014 and March 2022. It identified 51 false-negative exams for a rate of 0.8 per 1,000 screens.
Two radiologists then evaluated the false-negative exams. The women with the false-negative findings had an average age of 60 at diagnosis and the average time between screening and diagnosis was 7.1 months.
The researchers found that 35 of these cancers were indeed negative on DBT, while the remaining 16 were missed cancers. They also reported that extremely dense breast tissue was most frequently tied to true-negative cases at eight out of the 16 cases (p = 0.032). Following this was one-view findings (n = 6). Additionally, masses accounted for most of the missed mammographic findings at 14, with calcifications making up the remaining two cases.
Along with dense breast tissue and one-view findings, the team listed other contributing factors for missed cancers, each accounting for four or less of the missed cases. These included the following: developing asymmetries, distracting findings, postsurgical changes, benign-appearing masses, edge of image, patient positioning, very few calcifications, and poor image quality.
"Radiologists should be cognizant of these pitfalls to improve cancer detection on screening DBT," Zhou said.
A significant role
Breast density also played a significant role in the Bahl team's study, which focused on evaluating the characteristics of interval cancers. The researchers also found a false-negative rate of 0.8 per 1,000 DBT exams (110/143,622).
The team found that of the 110 women with false-negative cancers, 74 had heterogeneously dense or extremely dense breasts on mammography while the remaining 36 had a prior history of breast cancer.
The researchers also reported that 96 of the missed cancers were invasive malignancies, which had an average size of 15 mm. Of these cases with available data, 81.3% (74/91) were grade 2 or 3, 84% (79/94) were estrogen receptor-positive, and 35.3% (30/85) were lymph node-positive.
Additional imaging modalities and symptoms helped diagnose the false-negative cancers. Presented symptoms helped diagnose 60 (54.5%) of the cases, high-risk screening MRI detected 44 (40%), and other imaging modalities such as PET/CT detected five cases (4.5%). Elective prophylactic mastectomy incidentally diagnosed breast cancer in one case.
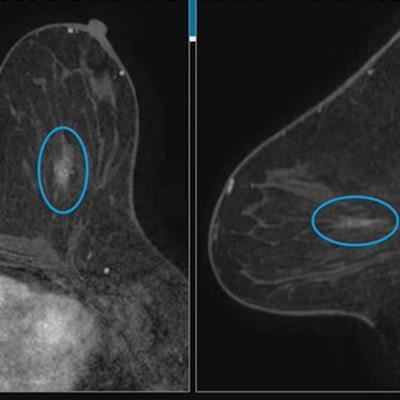
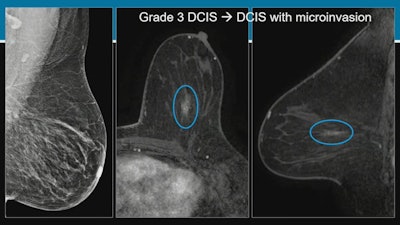 Researchers at the ARRS annual meeting described false-negative rates and characteristics on screening digital breast tomosynthesis (DBT). For these images, Dr. Manisha Bahl from Harvard Medical School described an asymptomatic false-negative case from a 53-year-old woman with a personal history of breast cancer. About 10 days after her initial screening, the woman underwent high-risk breast MRI which showed linear nonmass enhancement in the central area of the left breast. MRI-guided biopsy indicated grade-three ductal carcinoma in situ (DCIS), though this was upgraded to DCIS with microinvasion upon mastectomy. Images courtesy of ARRS.
Researchers at the ARRS annual meeting described false-negative rates and characteristics on screening digital breast tomosynthesis (DBT). For these images, Dr. Manisha Bahl from Harvard Medical School described an asymptomatic false-negative case from a 53-year-old woman with a personal history of breast cancer. About 10 days after her initial screening, the woman underwent high-risk breast MRI which showed linear nonmass enhancement in the central area of the left breast. MRI-guided biopsy indicated grade-three ductal carcinoma in situ (DCIS), though this was upgraded to DCIS with microinvasion upon mastectomy. Images courtesy of ARRS.Finally, the team reported that MRI-detected false-negative cancers were less likely to be invasive malignancies compared with symptomatic false-negative cancers. Of the 44 cases detected by MRI, 33 (75%) were invasive malignancies, compared with 58 (96.7%) of the 60 that were symptomatic false-negative cases on DBT (p < 0.001). Also, MRI-detected cancers were less likely to be lymph node positive (6/31) compared with symptoms (21/50, p = 0.04).
"Further research is needed to understand the role of supplemental screening with MRI in women at risk for interval cancers with DBT alone and to understand the impact of screening with DBT on long-term patient outcomes," Bahl said.
She added that the ongoing Tomosynthesis Mammographic Imaging Screening Trial (TMIST) will shed insight into whether DBT leads to a reduction in advanced breast cancers.