Minnies winners, page 2
Best Radiologist Training Program
Minnies 2022 Winner: University of Pennsylvania, Philadelphia, PA
The "heart and soul" of the University of Pennsylvania's (Penn) radiologist training program lies in its residents celebrating each other's accomplishments and leadership supporting tomorrow's radiologists, says Dr. Mary Scanlon, program director of Penn's diagnostic radiology residency program.
Perhaps it's these aspects that notched Penn its first Minnies award in the category of Best Radiologist Training Program. Or maybe it's the multiple education tracks the university offers for its radiology residents, including in teaching, business, and research, among others.
"We also train them to be leaders in their future academic or private practice careers over multiple domains," Scanlon said. "We want them to define the future of radiology."
While at Penn, residents learn not only the ins and outs of radiology, but also life skills such as collaboration and celebration. Although Philadelphia may seem large and intimidating for residents hailing from outside eastern Pennsylvania, Scanlon said residents go through personalized teaching sessions, team breakouts, small-group sessions, and dedicated minicourses. They also do out-of-classroom group activities such as pumpkin carving and blueberry picking.
"You don't have to be best friends with everybody, but we want to be a family and we want to take care of each other," Scanlon said. "You want to be in a program where your fellow residents will cover you if you need covering."
In their fourth year, residents have the opportunity to hone their skills and further develop their professional interests in their respective areas. Penn also has independent call shifts and a night float system. Through these, residents work on a diverse case mix from multiple hospitals in and associated with Penn Medicine.
To help with training, Penn Interventional Radiology has multiple suites for residents to use. These include one CT fluoroscopy suite, two C-arm suites, two procedural CT scanners, a preprocedure suite, and a large postprocedure recovery suite. The Perelman Center, meanwhile, has two C-arm suites, a venous ablation suite, and a dedicated interventional radiology clinic with four clinic rooms and provider workroom areas. Ultrasound is also available in all interventional suites and clinics.
Scanlon added that leadership reflects and acts on feedback from residents for their training program to help them get the most out of their education and personal interests. And with 100% employment and fellowship rates, Penn has the numbers to boot.
"We position our residents to reach for the stars and if they belly flop, we will be there to help them up," Scanlon said. "We don't want them to just be worker bees; we want them to be leaders. We also really promote the importance of organization and activism."
Runner-up: University of Wisconsin
Best Radiologic Sciences Training Program
2022 Minnies Winner: Thomas Jefferson University
Thomas Jefferson University (TJU) in Philadelphia has many educational resources and imaging technologies for residents to become successful in radiology, but it's the people who make the university's radiologic sciences training program successful, says program director Dr. Colleen Dempsey.

"The students, faculty, administration, and clinical affiliate partners work hard and remain dedicated to the success of our students and programs," Dempsey said.
This year's Minnies award marks TJU's fourth in this category, further adding to the institution's legacy. The university offers bachelor's and master's degrees in radiologic sciences, giving graduates more flexibility when entering the workforce. This includes a single-concentration track for 12 months or a dual-concentration track for 24 months for the bachelor's program. The curriculum integrates didactic, laboratory, and clinical education into its curriculum, and clinical rotations increase over time.
Among the university's other programs include a CT and PET/CT certificate, as well as two master's degrees in medical imaging and radiation sciences and in medical physics. Concentrations within the Department of Medical Imaging and Radiation Sciences are also offered in radiography, CT, MRI, invasive cardiovascular technology, nuclear medicine, radiation therapy, medical dosimetry, women's imaging, and other areas.
Dempsey added that the concentrations offer students the opportunity to train at clinical facilities that are leaders in healthcare and their communities.
"The department challenges, supports, and encourages our students to think and explore like they have never done before," she said. "The students learn from the diverse patient populations they care for and are able to be involved in experiences where they can apply clinical reasoning and thinking skills."
Equipment that students and faculty use include digital radiography x-ray rooms, a C-arm, mobile x-ray equipment, treatment planning systems, a virtual environment radiation therapy (VERT) lab, online simulation software for x-ray, MRI and CT, simulation OB/GYN sonography equipment, and multiple other ultrasound machines with a variety of software packages.
The university also prides itself on the program's 95% to 100% career placement rate since 1995, as well as the 85% pass rate on certification exams for all imaging concentrations. The program's attrition rate is less than 10%.
"The department ... does not operate in a silo. We are supported by so many people who are dedicated to the support and success of our students," Dempsey said. "I am proud of the team and look forward to continuing to positively contribute to student success which directly impacts the care of our patients."
Runner-up: Johns Hopkins University
Most Significant News Event in Radiology
Minnies 2022 winner: A shortage in the U.S. supply of contrast media
This year's Most Significant News Event in Radiology can be pinned to a date. On April 17, GE Healthcare notified customers to expect delays in supplies of its iohexol (Omnipaque) iodinated contrast media, as its production facility in Shanghai, China, had been shut down due to a local outbreak of COVID-19.
The crisis lasted for three months. Ultimately, the shortage exposed a weakness in the U.S. supply chain, limiting the ability to care for millions of patients and prompting radiology departments to make dramatic changes in imaging protocols and patient triage.
On May 4, the Greater New York Hospital Association signaled the scramble for contrast was on in an alert to member hospitals. Evaluate how much contrast you have on hand, and consider other imaging approaches over CT and x-ray, the organization suggested.
"Seek other means of securing contrast media, including alternate wholesalers and distributors," an official wrote.
On May 10, the ACR issued a statement that offered its recommendations for how to handle the situation, also highlighting the use of alternative studies, such as noncontrast CT, MR with or without gadolinium-based contrast, ultrasound with or without ultrasound contrast agents, or use nuclear medicine or PET/CT, when feasible.
This was followed on May 13 with a clinical perspective published by the American Journal of Roentgenology, which stressed the need for radiology departments to cut overall iodinated contrast media use through tactics such as direct dose reductions, using alternative imaging modalities or CT contrast agents, or delaying imaging.
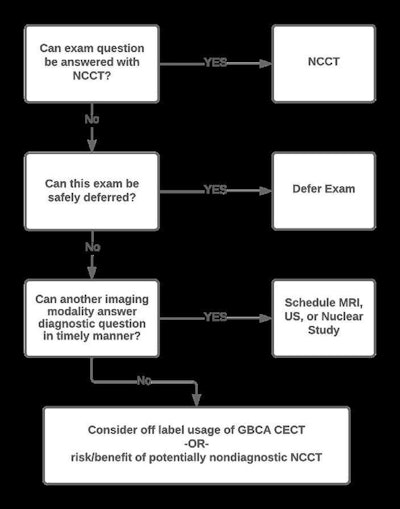
Alternative contrast agents such as iodixanol (Visipaque, GE) and ioversol (Optiray, Guerbet) also became scarce as practices shifted to using those products instead of iohexol.
By mid-May, GE's Shanghai production facility had ramped back up to 50% production and had shifted to delivery by air rather than by ship, which left some experts feeling optimistic. A group led by Dr. Thomas Grist of the University of Wisconsin in Madison encouraged a look at the larger picture.
"We must embrace this situation as a call to action to identify and correct other potential weaknesses in our supply chain that might limit our ability to care for the patients we serve," Grist told AuntMinnie.com.
Meanwhile, a group of interventional radiologists led by Dr. Nicole Keefe at the University of North Carolina (UNC) Medical Center in Chapel Hill, discussed their approach to the crisis, which included strategies for managing existing supply to minimize waste.
"From a diagnostic standpoint, all available imaging that could be changed to a different modality was changed," Keefe told AuntMinnie.com.
By June 9, modeling studies had been developed, with a team led by Dr. Michael Davenport of Michigan Medicine in Ann Arbor suggesting in JAMA that the use of intravenous contrast for CT exams can be reduced by more than 80% by combining dose-reduction strategies.
The shortage was mostly resolved by the end of June, with GE's Shanghai facility back to normal production. For its part, GE said at the time that it plans to remain proactive regarding its CT contrast capacity.
"We have invested almost $400 million over the past decade to increase production capacity in our manufacturing sites," a spokesperson told AuntMinnie.com. "Our focus is on restabilizing supply as availability improves."
Yet supply concerns have lingered, and one group of head and neck imaging experts explored whether MRI and ultrasound offer alternatives to CT with iodinated contrast in such crises as contrast shortages.
It's unknown how many patient procedures may have been affected by the shortage. Experts noted the crisis is likely to have a long-term impact in terms of how radiology departments and hospitals around the world stock contrast and where they procure it.
Ultimately, the crisis forced a hard look at how to avoid a similar disruption in the future, according to Davenport.
"I suspect it will be followed by a months-long introspection on the necessity of contrast for all exams for which it was previously used, the true required dose of contrast, and supply chain implications of the recent event," he said.
Biggest Threat to Radiology
Minnies 2022 Winner: Physician burnout
For the fourth straight year, the Minnies expert panel has selected physician burnout as the biggest threat to radiology.

Already an issue prior to COVID-19, the problem of burnout in radiology -- and in healthcare overall -- has only gotten worse during the pandemic. A recent survey found that one in four clinicians -- physicians, advanced practice practitioners, and nurses -- in the U.S. want to leave their career in healthcare, overwhelmingly due to burnout. And about one-third were considering moving to another employer.
Radiologists are being asked to do more with less, and over time, that dynamic often leads to burnout. And the problem is pervasive; one-third of radiologist leaders in private practice were found to be experiencing burnout. And it isn't just radiologists who are affected; radiology staff such as radiologic technologists have also experienced high rates of burnout. Some believe that the need to provide mental health support to radiologic technologists can't be overstated.
Not surprisingly, burnout can also affect patient care. Recent research found that patient safety incidents were twice as common among emergency physicians who considered themselves to be burned out.
Unfortunately, there is no easy fix for the problem. For example, a study published in August concluded that radiology department initiatives such as team-building events, more medical assistants, and an hourly cap on workdays failed to produce a measurable impact on the wellbeing of radiologists.
Some believe that instead of focusing on individual radiologists, efforts to prevent burnout should emphasize on the organizational level in order to foster a positive work culture and a sense of community and belonging. It's also important for leadership teams to be proactive about addressing burnout and show their employees that they care.
And artificial intelligence (AI) technology may also have a role to play in decreasing burden on radiologists and technologists. But one thing's for sure: the issue of burnout in radiology won't be going away any time soon.
Runner-up: Corporate takeover of independent radiology practices
Hottest Clinical Procedure
Minnies 2022 winner: Photon-counting CT
For the second year in a row, photon-counting CT has been selected by the Minnies panel as the Hottest Clinical Procedure. Ever since the U.S. Food and Drug Administration (FDA) cleared Siemens Healthineers' Naeotom Alpha photon-counting scanner in September 2021, the imaging world has been abuzz over how the technology can be used and how it benefits patients.
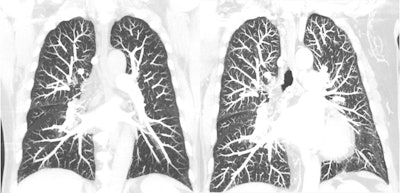
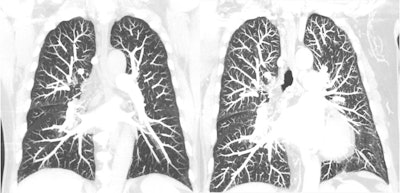 Coronal chest, with conventional CT with energy-integrating detectors (EIDs) on the left and photon-counting detector CT on the right. Courtesy of Cynthia McCollough, PhD.
Coronal chest, with conventional CT with energy-integrating detectors (EIDs) on the left and photon-counting detector CT on the right. Courtesy of Cynthia McCollough, PhD.Various teams of researchers have reported that photon-counting CT performs well across a variety of applications, from visualizing multiple myeloma and cerebrospinal fluid (CSF) venous fistula (CVF) better than conventional CT to helping to better diagnose interstitial pneumonia. Other vendors have thrown their hats into the proverbial photon-counting CT ring as well: In March, NeuroLogica secured FDA clearance for its mobile CT system with photon-counting detectors, and Canon Medical Systems, GE Healthcare, and Philips have indicated they are at full throttle in their own photon-counting CT development.
The technology's advantage over conventional CT is that it obtains images at a higher resolution but a lower radiation dose through a streamlined process in which x-rays are converted directly to electrons -- rather than CT's two-step process, which involves converting x-rays to light and then to an electronic signal. The limitation of this is that the light must be converted to a single pixel, which affects radiation dose efficiency and includes noise.
At the recent International Society for Computed Tomography (ISCT) meeting, Cynthia McCollough, PhD, of the Mayo Clinic in Rochester, MN, offered an overview on the technology and a comprehensive list of its benefits, which include the reduction of electronic noise, increased iodine contrast-to-noise/dose efficiency, higher iodine signal at high kV, better spatial resolution, lower radiation dose, and reduced beam hardening and metal artifacts.
"In addition to its astounding spatial resolution, photon-counting detector CT provides full time multi-energy capabilities," McCollough told AuntMinnie.com. "Users don't need to choose between ultra-high resolution and multi (dual)-energy."
Photon-counting CT has entered the clinical arena, according to McCollough.
"Decades of work by detector manufacturers, in conjunction with CT scanner manufacturers, have brought the field to the point where these systems are commercially viable," she said. "They are no longer just a research curiosity -- they are clinical CT systems."
Runner-up: Portable MRI