Body composition analysis of preoperative abdomen CT exams can opportunistically predict mortality in patients who have spinal metastases, according to research published online October 23 in the Spine Journal.
In a retrospective study involving nearly 200 patients, researchers from Massachusetts General Hospital and Harvard Medical School found that CT-determined sarcopenia was associated with a significantly higher risk of one-year mortality in these patients.
"This implies that body composition measurements such as sarcopenia could serve as novel biomarkers for prediction of mortality and may supplement other existing prognostic tools to improve shared decision making for patients with spinal metastases that are contemplating surgical treatment," wrote the team of researchers led by first author Dr. Michiel Bongers and corresponding author Dr. Miriam Bredella of Massachusetts General Hospital and Harvard Medical School.
Body composition measurements have recently been proposed as biomarkers for survival both in patients with and without cancer, according to the researchers. Hypothesizing that low muscle and abdominal fat mass were positive predictors of mortality, they sought to determine if body composition analysis on routine staging or therapy surveillance CT exams could opportunistically provide the first reliable predictor of survival in patients with spinal metastases.
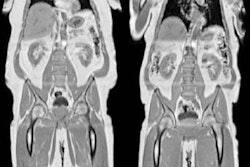
They first gathered data from 196 patients between 2001 and 2016 who had received surgical treatment for spinal metastases and had received a preoperative abdomen CT exam within three months of the surgery. Next, the researchers used an in-house automated software application to quantify the cross-sectional areas and CT attenuation of abdominal subcutaneous adipose tissue, visceral adipose tissue, as well as paraspinous and abdominal skeletal muscle. This analysis was performed on the CT images at the level of the L4 vertebrae.
Of the 196 patients, 76 (42%) had sarcopenia, which was determined by dividing the total muscle cross-sectional area by the height squared. Cutoff values of less than 52.4 cm2/m2 for men and less than 38.5 cm2/m2 for women were used to classify sarcopenia. Finally, the researchers then assessed the performance of the body composition measurements for predicting 90-day and one-year mortality.
Sarcopenia wasn't independently associated with 90-day mortality, but it was for one-year mortality.
| Increased risk from sarcopenia for 1-year mortality | ||
| Without sarcopenia | With sarcopenia | |
| 1-year mortality | 41% | 66% |
The presence of sarcopenia had a hazard ratio of 1.68 (p = 0.02). What's more, sarcopenia continued to be independently associated with mortality even when controlling for the prognostic modified Bauer score, yielding a hazard ratio of 1.58, according to the authors. The difference was also statistically significant (p = 0.03).
In other body composition findings, neither abdominal fat cross-sectional areas nor muscle attenuation was independently associated with mortality. However, the researchers said they also reconfirmed that decreased serum albumin, faster growth primary tumor histology group, a history of previous systemic therapy, impaired Eastern Cooperative Oncology Group (ECOG) performance status, and cervical metastases are associated with mortality.
"This study may serve as a pilot in evaluating these body composition measurements as potential markers to predict mortality," the authors wrote.