Artificial intelligence (AI) technology can add significant value in the practice of neuroradiology, especially in the areas of quantitative imaging, triage, and image reconstruction, according to a Monday session at the AHRA 2022 meeting in Phoenix.
"[AI] in quantitative imaging improves detection, quantification, standardization, and consistency across the board," said Dr. Lawrence Tanenbaum, director of MR, CT, and advanced imaging and medical director for the eastern region of imaging services provider RadNet. "Triage can accelerate care as well as improve outcomes. And [the use of AI in] image reconstruction is a patient-centered care move, [enabling] less time for patients on the table, better quality across the board, better efficiency, and a great response to this economic environment."
Deep learning can also be used to support automated image acquisitions in spine MRI, for example, guiding the scan position and scan planes in a more reproducible manner, he said.
Also, natural language processing (NLP) technology can have a big impact on quality, ensuring compliance with guidelines and monitoring of patient compliance with follow- up recommendations. Furthermore, NLP can be combined with computer-aided detection (CAD) software, reviewing reports and alerting radiologists if they may have missed findings on an image, he said.
NLP could even be used to adjust imaging reports to different levels of understanding, such as that of patients and referring physicians, Tanenbaum said. It can also capture AI findings and insert the results directly into the radiology report, and even write the report's conclusion for the radiologist.
Tools such as these can also improve standardization among radiologists, he said.
Segmentation
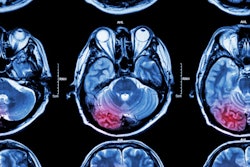
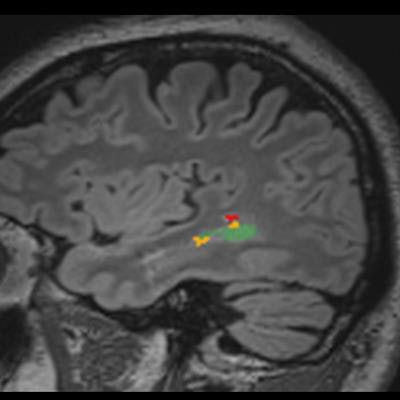
Segmentation is one of AI's natural capabilities and is useful in the brain and the spine, according to Tanenbaum. For example, AI can assist in assessment of multiple sclerosis (MS) by counting lesions and assessing change in both the size and number of lesions, he said.
"It isn't easy for a radiologist to tell whether a patient has 31 or 32 lesions," he said. "It's almost impossible. It's like counting spots on a Dalmatian."
There's also high inter-rater variability in counting of MS lesions.
"So using an AI-driven tool you can actually make the exam more efficient, balance out differences in expertise, and detect the differences and do it in a quantitative way," he said.
AI can also identify new lesions and show which lesions are bigger and which ones are smaller, Tanenbaum said.
"And that's very, very powerful," he said.
Several studies in the literature have shown that AI-assisted software for quantitative neuroimaging and MS can standardize and speed reporting, as well as enhance sensitivity.
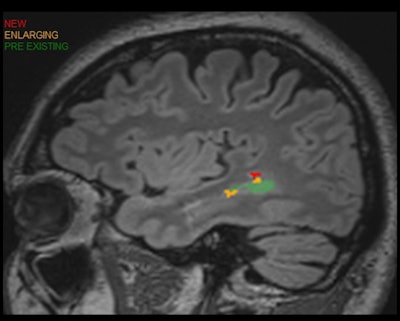 Patient with multiple sclerosis. Quantitative analysis enhances longitudinal analysis while increasing detection and efficiency. Image and caption courtesy of Dr. Laurence Tanenbaum and Icometrix.
Patient with multiple sclerosis. Quantitative analysis enhances longitudinal analysis while increasing detection and efficiency. Image and caption courtesy of Dr. Laurence Tanenbaum and Icometrix.Lesions changes can also be correlated with treatments on a report, enabling rapid assessment of treatment response.
"Using quantitative imaging, we were able to definitely identify that things were not working well, and with this information, leverage that and change therapy and ultimately improve outcomes," he said.
AI-based quantification also reduces both inter- and intra-rater variability, according to Tanenbaum.
Similar AI tools are available for assessment of traumatic brain injury, as well as dementia.
"One of the areas where volumetric imaging really took hold first is looking at dementia," he said. "By measuring certain structures in the brain, you can actually detect the classic phenotypes of different types of dementia."
This data can then be placed into a nomogram, providing an objective assessment and, perhaps, early detection of dementia at a phase when disease-modifying therapies could be applied, Tanenbaum said.
In spine imaging, AI is being used to assist in interpretation, reporting, and workflow, he said. It's also beneficial for localizing and labeling of spine structures and in segmentation. Other applications include deformity/scoliosis assessment, disc degeneration/Pfirman grading, and spinal stenosis evaluation.
Triage
Triage for urgent findings is perhaps the most common AI application in neuroimaging, with algorithms highlighting cases such as C-spine fracture or an intracranial hemorrhage for immediate review for radiologists, Tanenbaum noted.
Research has shown that these types of computer-aided triage tools have a quantitative impact on how quickly these studies are read, according to Tanenbaum.
"Triage tools are increasingly common and sometimes can make a difference in outcome and sometimes actually have reimbursement associated with it," he said.
Image reconstruction
AI is now taking over image reconstruction in CT, according to Tanenbaum. When used in image reconstruction, deep learning-based algorithms can maintain quantitative integrity while providing powerful denoising capability, according to Tanenbaum. In addition, it preserves or increases image sharpness or spatial resolution and also boosts contrast resolution and reduces artifacts, he said.
OEM vendors have also introduced or at least announced deep learning-based MR image reconstruction algorithms. And a vendor-agnostic tool is also available for MR image reconstruction from Subtle Medical, he said. Radnet is a partner of Subtle Medical.
As with CT, deep learning-based reconstruction maintains quantitative integrity and has powerful denoising capability for MRI, Tanenbaum said.
"Ultimately, it creates the ability to make a better image with greater sharpness, greater contrast to noise, and generally reduced artifacts," he said.
AI also enables high-quality images to be produced from significantly accelerated scanning protocols, sharply reducing MRI exam times.
Future developments
Looking ahead, efforts are currently underway to apply deep learning to produce synthetic image contrasts, using AI to reconstruct multiple contrasts from one scan, Tanenbaum said.
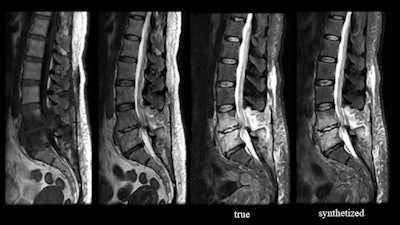 Osteomyelitis and discitis. Created using work-in-progress software from Subtle Medical, the synthetic image derived from the T1 and T2 images (left) emulates the true short tau inversion recovery (STIR) image. Images and caption courtesy of Dr. Laurence Tanenbaum and Subtle Medical.
Osteomyelitis and discitis. Created using work-in-progress software from Subtle Medical, the synthetic image derived from the T1 and T2 images (left) emulates the true short tau inversion recovery (STIR) image. Images and caption courtesy of Dr. Laurence Tanenbaum and Subtle Medical.AI may also help to address concerns regarding the use of gadolinium-based contrast agents. For example, Subtle Medical is developing SubtleGAD, a work-in-progress application that applies deep learning to synthesize post-contrast enhanced images from lower contrast-enhanced images. The software can generate images with 90% less gadolinium dose that look very much like a full-dose image, according to Tanenbaum.