CHICAGO -- Researchers have developed an AI model using PET scans that can identify metastatic neuroendocrine tumors (NETs) that are not responding to treatment, according to research presented December 3 at RSNA.
Sebastian Salgado-Maldonado, a doctoral student in medical physics at the University of Wisconsin-Madison, explained that the model has potential as a complement to treatment, given that patients with metastatic NETs typically exhibit heterogeneous lesion-level responses.
"We developed an accurate methodology for lesion-level response prediction,” he said. Sebastian Salgado-Maldonado presented an AI model at RSNA December 3 that could be useful in patients with metastatic NETs.
Sebastian Salgado-Maldonado presented an AI model at RSNA December 3 that could be useful in patients with metastatic NETs.
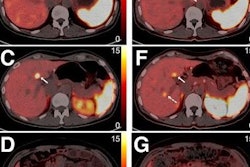
Metastatic NET patients have heterogeneous lesion-level responses to peptide receptor radionuclide therapy (PRRT), for instance, which means that individual metastatic lesions within the same patient respond differently to the same treatment. Some may shrink and others may progress.
While locoregional approaches such as trans-arterial embolization and stereotactic body radiation therapy are effective in managing non-responding NETs, selecting which metastatic lesions to target remains challenging, Salgado-Maldonado noted.
“What if we could predict the long-term lesion-level response?” he said.
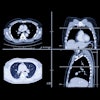
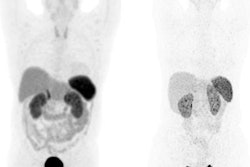
To that end, Salgado-Maldonado and colleagues tested whether machine learning and longitudinal PET-based tracking of individual lesions could help identify which metastatic NET lesions are likely to persist and benefit from locoregional treatment.
The researcher trained and validated a neural network on gallium-68 (Ga-68) DOTATATE PET images that included 423 lesions from eight metastatic NET patients, and then tested it on PET scans that included 116 lesions from five patients. Patients underwent PET scans at three time points: one week before the first PRRT cycle, 16 weeks post-treatment, and 65 weeks post-treatment.
An expert clinician segmented all lesions in the PET scans across all timepoints. The researchers extracted nine quantitative PET features -- mean standard uptake value, median, maximum, minimum, variance, skewness, kurtosis, volume, and total uptake for each lesion. With this input, the model was trained to predict which lesions persisted on the 65-week post-treatment PET scans.
On the training set, the model achieved an area under the curve (AUC) that varied between 0.77 when using one of the nine PET features to 0.79 when using three of the nine PET features. The maximum AUC of 0.79 was obtained when both the baseline and post-treatment data were used in the predictive model, Salgado-Maldonado noted.
Finally, on the test data of 116 lesions from five patients, the model achieved an AUC of 0.81, an accuracy of 80%, a sensitivity of 74%, and a specificity of 84%.
“Metastatic NET lesions that do not respond favorably to PRRT in the long term can be predicted using a fully connected neural network classifier,” Salgado-Maldonado said.
Ultimately, longitudinal information from both baseline and early post-treatment imaging was critical for the model’s optimal performance, he noted. Further development of the model is necessary, but Salgado-Maldonado said that eventually it could prove useful for providing clinical decision support in patients undergoing stereotactic ablative radiotherapy after PRRT or retreatment with PRRT.
Moreover, the group developed the model to be generalizable to other solid tumors, such as prostate cancer and melanoma, Salgado-Maldonado added.
“This methodology enables lesion-specific management of metastatic neuroendocrine tumors for partial responders and is readily extendable to other types of solid tumors,” he concluded.
For full coverage of RSNA 2025, visit our RADCast.