Congenital Lesions of the Thyoid Gland
Congenital hypothyroidism refers to hypothyroidism that is present at birth [3]. There is a slight female predominance (3.2:1) [3]. Thyroid dysgenesis (aplasia, hypoplasia, ectopia) is the most common etiology- accounting for about 80% of cases [3]. Instances of thyroid aplasia secondary to I-131 in utero exposure have been documented [3]. Infants with thyroid aplasia have a less favorable long-term prognosis [3].
Dyshormonogenesis refers to congential hypothyroidism secondary to one of several hereditary enzyme deficiencies resulting in defective thyroxine (T4) synthesis [3,4]. This etiology accounts for about 10-15% of cases of congenital hypothyroidism [3]. The enzyme defect or deficiency may occur anywhere, but the most common abnormality is an organification defect related to a absent or insufficient thyroid peroxidase resulting in failure to oxidize (organify) iodide to iodine and therefore binding to thyroglobulin cannot occur [3]. Cases of enzymatic defects of thyroid hormonogenesis demonstrate an autosomal recessive pattern of inheretance [3].
Causes of transient congenital hypothyrooidism include the presence of maternal antibodies due to a thyrotropin receptor blocking antibody that suppresses gland function [4]. Thyroid function recovers when once the antibodies are catabolized from the infants circulation [4]. Excess fetal or neonatal blood iodine will suppress thyroid hormone synthesis and this can occur as a result of iodine containing medications (such as povidone iodine), skin antiseptics or IV contrast agents (by either the mother or the neonate) [3,4].
Endemic cretinism secondary to maternal dietary deficiency of iodine accounts for less than 1% of cases of congenital hypothyroidism in the USA [3]. When present, a palpable goiter suggests an etiology of dyshormonogenesis or endemic cretinism [3]. Idiopathic pituitary aplasia (leading to TSH deficiency) or congenital midline brain defects such as septo-optic dysplasia may also produce hypothyroidism [3].
Combined use of nuclear medicine thyroid imaging and thyroid ultrasound provide the best means to evaluate neonates with hypothyroidism [4]. In 14-15% of cases in which the nuclear medicine scan demonstrates no thyroid uptake (a finding suggestive of dysgenesis), a normal thyroid gland can be seen at US [4].
Dyshormonogenesis/Organification Defect
Dyshormonogenesis results from a deficiency or absence of one or more of the enzymes involved in thyroid hormone synthesis or secretion. The most common enzyme abnormality is absent or insufficient thyroid peroxidase activity which results in failure of oxidation (organification) of iodide to iodine. With this type of defect iodine will be trapped, but not organified. Patients with peroxidase deficiency frequently have an enlarged gland (although it may be normal sized), an elevated TSH (due to decreased levels of circulating thyroid hormone), and a high uptake of I-123 (at 4 hours) and Tc-pertechnetate. T4 and FTI are usually decreased. The perchlorate washout test will be positive in these patients. Deficient peroxidase activity associated with a familial goiter and deafness or hearing loss is referred to as Pendred's syndrome.
Ectopic Thyroid Tissue/Thyroid Dysgenesis:
Ectopic thyroid tissue can be lingual, substernal, or pelvic/ovarian teratoma (struma ovarii). Pertechnetate is generally not useful for imaging the substernal area due to attenuation or superimposed blood pool activity.
Lingual Thyroid
The point of origin of the thyroglossal tract is the foramen cecum which lies at the vertex of the sulcus terminalis linguae at the base of the tongue [6]. A lingual thyroid occurs due to an extreme failure of thyroid migration. The base of the tongue is the most frequent site of ectopic thyroid tissue - accounting for as many as 90% of cases [6]. The gland may provide adequate amounts of thyroid hormone, or may fail in early childhood (15-30% of cases). In 70-80% of patients with a lingual thyroid, no other thyroid tissue can be found in the neck [1,6]. If ectopic tissue is present, it can produce an enlarging midline/upper neck mass as a result of hyperstimulation which clinically resembles a thyroglossal duct cyst. Symptoms are typically related to mass effect and include dysphagia and dyspnea. There is an association with thyroglossal duct cysts.
|
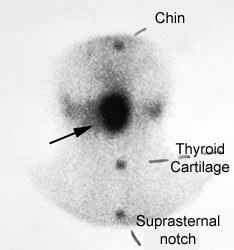
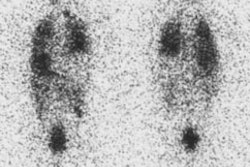
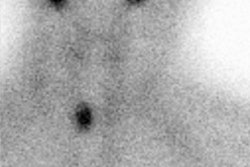
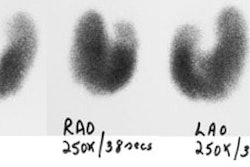
Lingual thyroid: The patient below presented for evaluation of a midline neck mass. The Tc-pertechnetate exam demonstrated the abnormality to be due to a lingual thyroid. No normal thyroid tissue can be seen in the thyroid bed. |
|
|
Thyroglossal duct cyst
Thyroglossal duct cysts appear in the midline along the migratory
path of the embryologic thyroid gland, anywhere from the foramen
cecum at the base of the tongue to the lower neck. They are found
in the suprahyoid neck in 25% of cases, at the level of the hyoid
in 15-50% of cases (most common location), and below the hyoid in
20-65% of cases (infrahyoid TDCs may have a median or paramedian
location and may be embedded in the strap muscles of the neck)
[2,7].
There is no gender predilection [2]. About half of the patients
present before the age of 20 years with an enlarging, painless,
mid-line mass [2]. On clinical exam, a thyroglossal duct cyst will
typically move vertically with protrusion of the tongue or
swallowing, which confirms a relationship between the two
structures [6,7]. The cyst may become infected, and rarely a
papillary thyroid carcinoma may develop within a thyroglossal duct
cyst (less than 1% of cases [2]). Treatment is surgical resection,
but prior to treatment a properly positioned normal thyroid gland
must be confirmed [7].
US will show a hypo- or anechoic cystic structure [2,7].
Heterogeneity (septa, debris, or internal echos) can be seen due
to the proteinaceous content or hemorrhage within the mass [2,5].
A soft tissue mass associated with a TDC may represent ectopic
thyroid rests, or rarely a thyroid cancer [7]. At CT, the cyst
appears as a well circumscribed, thin walled mass with mucoid
attenuation (0-20 HU) [2,5]. Peripheral rim enhancement can be
seen following contrast administration [2]. On MR, uncomplicated
cyts with have low signal on T1 and high signal on T2 [2]. If the
fluid within the cyst is proteinaceous or hemorrhagic the lesion
can have higher signal on T1 images [5].
The vast majority of patients with thyroglossal duct cysts have
normal thyroid scans. Surgery is contraindicated if functioning
thyroid tissue is demonstrated in the mass.
Substernal Thyroid
I-123 is the preferred imaging agent due to mediastinal blood pool activity with Tc-99m. Most intrathoracic goiters demonstrate anatomic continuity, but not necessarily functional continuity with cervical thyroid tissue.
Hemiagenesis
Females are affected more than males (3:1). The left lobe of the gland is absent in about 80% of the cases [1]. The remaining lobe is hypertrophied, but normal in shape [1].
REFERENCES:
(1) Thyroid and whole-body imaging. Charkes ND. In The Thyroid, 5th ed. Ed Ingbar and Braverman. Lippincott, Philadelphia, 1986. 458-478
(2) Radiographics 2005; Meuwly JY, et al. Multimodality imaging evaluation of the pediatric neck: techniques and spectrum of findings. 25: 931-948
(3) Pediatr Radiol 1986; Wells RG< et al. Technetium 99m pertechnetate thyroid scintigraphy: congenital hypothyroid screening. 16: 368-373
(4) Radiology 2011; Chang YW, et al. Congenital hypothyroidism:
analysis of discordant US and scintigraphic findings. 258: 872-879
(5) Radiographics 2011; Fang WS, et al. Primary lesions of the
root of the tongue. 31: 1907-1922
(6) Radiographics 2014; Zander DA, Smoker WRK. Imaging of ectopic
thyroid tissue and thyroglossal duct cysts. 34: 36-50
(7) Radiographics 2018; Bansal AG, et al. US of pediatric
superficial masses of the head and neck. 38: 1239-1263