Behcet's Disease:
Clinical:
Behcet's disease is a chronic multisystem vasculitis of unknown
etiology that may affect the lung in 5 to 8% of patients
(typically in the late stage of the disorder) [1,2]. The condition
primarily affects young men (second or third decade) from
Mediterranean countries, the middle East, or Japan [2]. However,
other authors indicate an equal male-female involvement [1]. The
diagnosis is consists of the presence of recurrent oral
ulcerations plus two additional criteria including recurrent
genital ulcerations, eye lesions (uveitis), skin lesions, and
positive pathergy tests [2,4]. The reported prevalence of thoracic
involvement in Bechet's disease ranges from 1-8% [4]. The disorder
can involve large, medium, and small arteries, as well as the
venous circulation [1] (venous thrombotic disease is a predominant
feature, whereas arterial involvement is substantially less
frequent [6]). Systemic arterial manifestations of the disorder
are infrequent in comparison to venous involvement [1]. The aorta
in the most commonly involved artery, followed by the pulmonary
arteries [4].
Pulmonary involvement can occur in up to 18% of cases [6].
Pulmonary artery involvement can result in vessel occlusion or
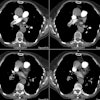
more commonly, an aneurysm [3]. Pulmonary artery aneurysms (or
pseudoaneurysms) occur in about 1.1% of patients [1]. They
aneurysms are commonly multiple, bilateral, saccular, and involve
the lower lobe or main pulmonary arteries [1]. The aneurysms are
frequently partially or completely thrombosed [4].
The presence of pulmonary artery aneurysms suggests a poor prognosis in untreated patients- with a mortality rate of up to 30% within 2 years [2,4]. Selective transcatheter embolization can be used for therapy [2]. Up to 75% of aneurysms may resolve when patients are treated with immunosuppresant therapy [4].
X-ray:
Radiologic findings include the presence of an aneurysm that can appear as a focal mass [5]. Perianeurysmal air-space consolidation or GGO is indicative of an impending rupture [5]. Vessel wall thickening can be seen in the aorta and superior vena cava [4]. SVC thrombosis and thrombosis of other mediastinal veins is not uncommon [4]. Parenchymal lung findings include subpleural alveolar infiltrates and wedge-shaped area of increased opacity that represent focal vasculitis and thrombosis of pulmonary vessels resulting in infarction, hemorrhage, and focal atelectasis [4].
REFERENCES:
(1) AJR 2005; Marten K, et al. Pattern-based differential diagnosis in pulmonary vasculitis using volumetric CT. 184: 720-733
(2) Radiographics 2005; Pelage JP, et al. Pulmonary artery interventions: an overview. 25: 1653-1653
(3) Radiographics 2006; Castaner E, et al. Congenital and acquired pulmonary artery anomalies in the adult: radiologic overview. 26: 349-371
(4) Radiographics 2010; Castaner E, et al. When to suspect pulmonary vasculitis: radiologic and clinical clues. 30: 33-53
(5) Radiology 2010; Chung MO, et al. Imaging of pulmonary
vasculitis. 255: 322-341
(6) AJR 2013; Nemec SF, et al. Noninfectious inflammatory lung disease: imaging considerations and clues to differential diagnosis. 201: 278-294