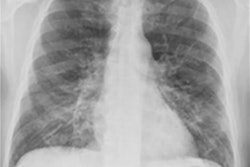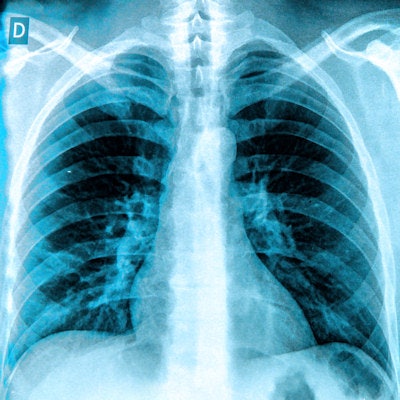
Researchers have developed a scoring tool for chest x-rays that can be used to predict outcomes for patients diagnosed with COVID-19, according to a study presented April 15 at the 2021 American Roentgen Ray Society (ARRS) virtual annual meeting.
The study identified laboratory, clinical, and radiographic data in chest x-rays that predicted important COVID-19 patient outcomes, such as death, intubation, and the need for chronic renal replacement therapy (CRRT). The tool was effective in settings of a high pretest probability of COVID-19 infection and can be used both at the attending chest radiologist and junior resident levels, according to the researchers.
"These findings are supported by prior work, validating the utility of [chest x-ray] for patient prognostication, while adding new insight into COVID-19 infection during the initial presentation," wrote the group led by Dr. Russell Reeves of Thomas Jefferson University in Philadelphia.
In the study presented at ARRS, Reeves and colleagues identified 240 patients (142 males, 98 females; median age, 65 years) with confirmed COVID-19 who were admitted to an urban multicenter health system from March 16 to April 13, 2020. Three cardiothoracic radiologists and three diagnostic radiology residents independently scored their admission chest x-rays, based on extent and severity of COVID-19 pneumonia. Demographic variables, clinical characteristics, and admission laboratory values were collected, while interrater reliability among attendings, residents, and the combined group of graders was assessed.
Reliability for the chest x-ray scoring was a mean of 0.686 among the attendings, residents, and combined group who used it. They identified no difference in outcomes across gender, race, ethnicity, or those with either a history of lung cancer or chronic obstructive pulmonary disease.
Although chest x-ray severity proved an independent predictor of death (p < 0.001), severity was a nonindependent predictor of CRRT (p = 0.007) and intubation (p < 0.001), but not extracorporeal membrane oxygenation, the authors concluded.