Without the beneficence of academia, or initially even the blessing of gastroenterologists in their own facility, radiologists in Belgium have built a popular virtual colonoscopy (VC or CT colonography [CTC]) practice they credit with increasing awareness of colorectal cancer screening in their community and reducing unnecessary optical colonoscopies. The screening model offers a glimpse of what U.S.-based community screening practice might look like with a bit of reimbursement.
Since 2003, Dr. Danielle Hock and her team at Clinique St. Joseph CHC in Liège have performed nearly 5,000 virtual colonoscopies, with high accuracy and relatively low numbers of referrals to optical colonoscopy. In Belgium, screening VC is reimbursed as a regular abdominal CT exam.
The first patients were referred for double-contrast barium enema and their exams simply switched to VC, "but now our indications are very broad," Hock said. Primary care providers provide nearly all the referrals, with only 5% referred by gastroenterologists, she said.
"We began slowly but at the present time we see 10 to 15 patients three times per week" using just two radiologist readers, Hock said at the 2007 International Symposium on Virtual Colonoscopy in Boston. Of necessity, throughput is very efficient.
On exam days, one patient is positioned in the scanner while another waits for the results to be read.
"Patients are asked to wait in the waiting room, still fasting, before hearing the results," she said. "In case of positive findings, we propose image-guided resection (via colonoscopy), depending of course on the age and condition of the patient," she said. Same-day colonoscopy was not performed during the first two years "because at the beginning of our practice the gastroenterologists at our institution simply refused," she said.
After following a clear liquid diet, patients undergo cathartic bowel cleansing (generally using sodium phosphate bisacodyl tablets, or alternatively magnesium phosphate or polyethylene glycol), fluid tagging by ingestion of dimeglumine gadopentetate (Gastrografin, Bracco, Milan), and automated insufflation with CO2 (ProtoCO2l, E-Z-EM, Lake Success, NY).
Then prone and supine images are acquired on a 32-slice scanner (VCT LightSpeed, GE Healthcare, St. Giles U.K.) using collimation of 0.675 mm and 1.25-mm overlapping reconstructions.
The group uses GE's AutoDissection application, which automatically locates the start and end of the colon to create a "virtual dissection" view. For the past two years, interpretation has also included concurrent reading with computer-aided detection (Colon VCAR, GE Healthcare), an application that uses pattern-matching algorithms to locate suspicious regions in the colonic mucosa.
Even under the most carefully controlled circumstances, absolute sensitivity and specificity cannot be reported in patients whose VC results did not lead to subsequent optical colonoscopy. And unfortunately for her results, Hock said, accuracy was compromised even for patients who underwent both exams by the gastroenterologists' incomplete recordkeeping with regard to the size, number, and location of detected lesions.
On the radiology side, "we committed the mistake during our first two years of reporting 4- to 5-mm lesions," which led to biases in the number of small lesions reported during this time, she said. These 4- to 5-mm lesions reported at VC during the first two years accounted for 32 of 58 false positives during that period when they were not confirmed at conventional colonoscopy.
 |
| A 74-year-old asymptomatic woman presented for screening virtual colonoscopy. Findings confirmed at optical colonoscopy included two tubulous adenomas in the sigmoid colon. Lumen view image courtesy of Dr. Danielle Hock. |
The patients' mean age was 59.9 years (42% men, 58% women; ages 17-93). Twelve percent of the patients had a personal or family history of colorectal cancer, 7% presented with anemia or active bleeding, 53% had a change in bowel habits or abdominal pain, and 28% were asymptomatic subjects presenting for screening.
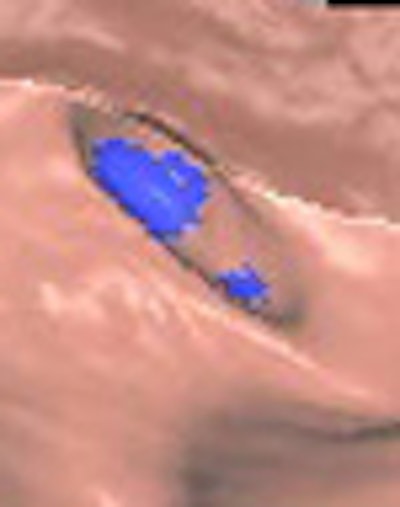
 |
| A 73-year-old woman presenting with diarrhea underwent virtual colonoscopy. Findings confirmed at conventional colonoscopy included a tubulovillous tumor in the rectum, juvenile polyp in the sigmoid colon, and tubulovillous tumor above the ileocecal valve. 3D endoluminal image courtesy of Dr. Danielle Hock. |
In all, 295 of the 4,655 (7.5%) patients with negative findings at VC underwent optical colonoscopy, which in many early cases was not indicated and "proved to be true-negative in 97% of the cases," she said. Among all patients, "there was around 3% of false negatives (at VC), including three tumors, one large polyp, and two intermediate-sized polyps." Among detections at VC, 86% were true-positive and 14% false-positive at colonoscopy, including one tumor and six large polyps.
VC findings matched those of optical colonoscopy in 287 of 375 (76%) cases, she said, including 19 normal colons with at least a single medium-sized polyp (6-10 mm). Among the remaining 88 patients, four (1%) were false-negative at colonoscopy, and 84 (23%) were deemed false-positive. Thirteen percent of all findings were tumors, 19% were large polyps (> 10 mm), 35% were intermediate-sized lesions (6-10 mm), and 33% were small polyps (< 6 mm). The positive and negative predictive values of virtual colonoscopy for detecting patients with significant lesions were 86% and 97%, respectively.
 |
| VC results showed per-patient sensitivity and specificity of 98% and 83% for detecting significant lesions. Positive and negative predictive values were 86% and 97%, respectively. Chart courtesy of Dr. Danielle Hock. |
Given the stated limitations of the methods and documentation, particularly during the first two years of practice, the overall reported sensitivity and specificity of 98% and 83%, respectively, for clinically significant polyps are almost certainly "too good to be true," Hock cautioned. But wherever the absolute truth might lie, she added, "the results are certainly very nice."
"When we reached our 1,000th study, we made a public announcement that we had routine practice for CTC in order to screen healthy patients," Hock said. "It was a real success, and we almost tripled the number of patients. Over those four years, the number of patients screened with CTC has increased, but also the number of patients screened with optical colonoscopy. In comparison with the number of polyps which are resected in our institution, the very slow augmentation means that we are just now screening (more) average-risk patients."
The percentage of referrals to optical colonoscopy after VC is acceptably low in average-risk patients, and the yield of colonic polyps and carcinomas in secondary referrals from virtual colonoscopy exceeds 70%, Hock said. Given the low prevalence of polyps in an average-risk population, the use of virtual colonoscopy could significantly reduce the number of nontherapeutic optical colonoscopies.
"CTC in routine practice is feasible and successful in a nonacademic institution with good results," she said. "Patient screening is increasing progressively for both optical and virtual colonoscopy, which is a good thing. And we are screening patients who had been reluctant to undergo optical colonoscopy. Indeed, after the age of 50, any abdominal symptom could be an easy opportunity to talk about colorectal cancer screening."
The study is ongoing, and the group hopes to publish updated results in 2008, Hock told AuntMinnie.com.
By Eric Barnes
AuntMinnie.com staff writer
December 21, 2007
Related Reading
Two-tier fecal occult blood screening offers effective colorectal cancer detection, October 30, 2007
Italian multicenter VC trial screens higher-risk cohort, October 17, 2007
Positive trial results boost VC's prospects for broader screening role, October 16, 2007
ACRIN trial shows VC ready for widespread use, September 28, 2007
Immunochemical test most sensitive for detecting colon cancer, September 26, 2007
Copyright © 2007 AuntMinnie.com




















