Double reading of MRI examinations in women with high risk of breast cancer can reduce the number of unneeded biopsies, decrease false-positive results, and improve detection of malignancies, according to research presented recently at the Canadian Association of Radiologists annual meeting.
Previous research has shown that double reading of mammograms by a second radiologist reduced recall rates and increased cancer detection, explained Dr. Jason Chan, a fourth-year resident in radiology at the Ottawa Hospital in Ontario, Canada, and presenter of the study (Radiology, June 2018, Vol. 287:3, pp. 749-757).
Other research, however, suggests that double reading does not offer a benefit over single reading with respect to the rate of cancer detection and that it is not cost-effective in the context of digital mammography (Plos One, July 26, 2016, Vol. 11:7, p. e0159806).
The radiology community has also been resistant to implementing double reads into examination workflow.
"There are concerns about double reads being more time consuming," Chan told AuntMinnie.com in an interview.
Beginning in October 2019, a policy of requesting a second read whenever a case warranted a biopsy was implemented at the Ottawa Hospital.
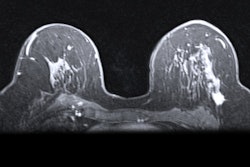
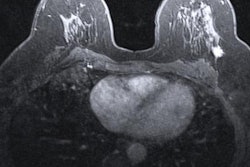
"This [process] was an institutional change at our center," Chan explained. "A radiologist would read a breast MRI scan, and if they thought that the patient needed a biopsy, they would inform a second radiologist to ask for their opinion."
To expedite communication between radiologists, the hospital used a secure chat function where a message containing the breast MRI scan and clinical judgment would be stored.
"Otherwise, the first reader would have to find the second reader in person and show them the scan," Chan said. "With our secure chat function, the radiologist receives a message that the examination has been done. The second reader's opinion could then be obtained right away."
In this investigation, Chan and colleagues compared a one-year period, June 1, 2018, to June 1, 2019, without double readings of breast MRI examinations to a subsequent one-year period, October 31, 2019, to October 31, 2020, with double readings of breast MRI examinations at the Ottawa Hospital. The researchers compared their outcomes with the Breast Imaging Reporting and Data System (BI-RADS) 5th edition breast MRI screening benchmarks.
All patients included in the retrospective, population-based cohort study were women between the ages of 30 and 69 who had a 25% or greater lifetime risk of breast cancer.
The outcomes of the study were abnormal interpretation rate and cancer detection rate, positive predictive value of recommendations for tissue diagnosis, and positive predictive value of biopsy performed. The investigators performed 1,124 screening breast MRI scans in the prepolicy period and 1,672 screening breast MRI scans in the active phase of the policy.
Significantly fewer biopsies were recommended when double reads of breast MRI screens were an option. Biopsies were recommended in 8.6% (97/1124) of exams in the prepolicy period, and they were recommended in 5.5% (92/1672) of breast MRI scans (p = 0.0012) once the policy was in place.
"There were significantly fewer biopsies recommended as a result," Chan noted.
In addition, there was no difference in the rate of cancer detection between the prepolicy period and active policy period. A total of 10 out of 1,124 (8.9/1,000) cancers were diagnosed in the prepolicy period and 17 out of 1,672 (10.2/1,000) cancers were diagnosed in the active policy period, yielding a nonsignificant p-value of 0.736.
There was a rise in the positive predictive value of recommendation for tissue diagnosis or biopsy from the prepolicy period (10.3%, 10/97) to active policy implementation (18.4%, 17/92), but it did not reach statistical significance (p = 0.109). Similarly, there was a rise in the positive predictive value of biopsy performed from the prepolicy period (14%, 10/71) to the active phase (22.9%, 17/74), which was also not significant (p = 0.17).
The increases did, however, meet the American College of Radiology (ACR) BI-RADS benchmarks. The increase in the positive predictive value of recommendation for tissue diagnosis to 18.4% meant it surpassed the ACR BI-RADS benchmark of 15%, Chan noted. The rise in the positive predictive value of biopsy to 22.9% meant that it fell within the ACR BI-RADS benchmark of between 20% and 50%. Investigators reported a decrease in abnormal interpretations from the prepolicy period (17.7%) to when the policy was active (14.5%, p = 0.022).
"Essentially, there were fewer false positives," said Chan, referring to the drop in abnormal interpretations. "That brings a lot of benefit as well. It means decreased patient anxiety."