Pulmonary Artery Pseudoaneuyrsm/Aneurysm:
Clinical:
Pulmonary artery pseudoaneurysms (PAPs) can occur as a result of erosion of the artery by an adjacent tuberculous cavity (Rasmussen aneurysm), infection, blunt or penetrating thoracic trauma, neoplasms, improper placement of flow directed pulmonary arterial (Swan-Ganz) catheters, and septic emboli (endocarditis). Hemoptysis is common. Causes of pulmonary artery aneurysms include Behcet's disease [4], Hughes-Stovins syndrome, and Marfans syndrome. [3]In one study, PAPs showed a strong predilection for the peripheral pulmonary artery branches with 83% located in the segmental or subsegmental branches [5]. The lesion tends to be solitary, but multiple lesions can be seen in association with endocarditis (septic emboli) and metastatic disease to the lung [5]. Massive hemoptysis may occur after rupture of a pulmonary artery pseudoaneurysm and is associated with a mortality rate as high as 50% [5]. Endovascular treatment by direct coil embolization, stent placement, or embolization of the feeding vessel are considered the treatment of choice [5].
i) Rasmussen (Tuberculous) Pseudoaneurysm:
Pseudoaneurysms are found in about 4% of patients with chronic cavitary tuberculosis at autopsy. Patients typically present with massive hemoptysis (over 300 mL/24 hr), but it is most commonly secondary to bronchial artery pseudoaneursym. Treatment is coil or balloon embolization [1].ii) Complications of Swan-Ganz catheterization:
A false aneurysm of the pulmonary artery may rarely occur as a result of peripheral placement of the catheter (about 0.15% of cases). The pseudoaneurysm typically forms following rupture of the vessel by the catheter. Generally, the right pulmonary artery is involved (93% of cases)- and typically the lesion occurs in a lower or middle artery. The rate of hemorrhage associated with a false aneurysm is between 30-40% and mortality is between 40-100% (mortality is increased following rupture of the pseudoaneurysm). Risk factors associated with pulmonary artery rupture include technical errors, anticoagulation, pulmonary arterial hypertension, long-term steroid therapy (fragile vessels), age greater than 60 years, and female sex. Technical errors can be avoided by inflating the balloon in a large pulmonary artery before pushing it distally and deflating the balloon before withdrawing it. Hemoptysis is the typical presenting symptom.X-ray:
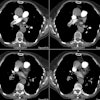
Following pulmonary artery rupture chest radiographs typically demonstrate an infiltrate which represents an area of hemorrhage. A false aneurysm may be detected as the infiltrate (hemorrhage) clears- leaving a rounded nodule or mass. CT with contrast will demonstrate the false aneurysm as an enhancing mass with an adjacent vessel and sometimes a partially thrombosed lumen. Percutaneous transcatheter embolization is the treatment of choice for a pulmonary artery false aneurysm. [2] However, the procedure can be complicated by pulmonary infarction following improper coil placement [3].REFERENCES:
(1) Radiology 1994; 193: 396-98
(3) AJR 1997; Hubler B, et al. Traumatic pulmonary arterial and venous pseudoaneurysms. 169: 1354 (No abstract available)
(4) AJR 1999; Tunaci M, et al. CT findings of pulmonary artery
aneurysms
during treatment for Behcet's disease. 172: 729-733
(5) AJR 2017; Chen Y, et al. Pulmonary artery pseudoaneurysms:
clinical features and CT findings. 208: 84-91