Coupling the radiopharmaceutical gallium-68 (Ga-68) prostate-specific membrane antigen (PSMA) with PET/CT or PET/MRI has been a boon for prostate cancer imaging. But clinicians still need to be aware of some inherent shortcomings with the radiopharmaceutical, according to a research review published online April 12 in Urology.
PET/CT and PET/MRI with Ga-68 PSMA are being used for staging and restaging of intermediate- to high-risk primary prostate cancer, and to guide and monitor response to therapies. Much of the available research has targeted the efficacy of Ga-68 PSMA PET with CT or MRI in different clinical situations with quite promising outcomes. Still, there are nuances to the use of Ga-68 PSMA that can cloud results.
"Both methods have become, in a relatively short period of time, the gold standard for restaging recurrent prostate cancer in those countries and clinical centers where these imaging modalities are available," wrote the German researchers led by Dr. Manuela Hoffmann from Johannes Gutenberg-University Mainz. "Their potential to facilitate more accurate prostatic biopsy, to guide therapy, and to monitor the therapeutic response to all treatment modalities is currently under intense investigation."
The severity of prostate cancer runs the gamut from "innocuous to aggressive and lethal," the authors noted, which is why "an accurate assessment of tumor characteristics is crucial for appropriate treatment."
Multiparametric MRI has become the gold standard for prostate imaging -- with T2-weighted, diffusion-weighted imaging (DWI), and dynamic contrast-enhancement (DCE) protocols greatly improving diagnostic accuracy, and with negative predictive values as high as 98% in some previous research. In addition, Ga-68 PSMA has shown promise when coupled with PET and PET/CT for prostate cancer staging and restaging.
Among the radiotracer's attributes are a long half-life of approximately 68 minutes and an ability to distinguish between low- and high-grade carcinoma in primary prostate cancer, with reported sensitivity of 84% and specificity of 100%. Curiously, the diagnostic accuracy of Ga-68 PSMA PET/CT and/or Ga-68 PSMA PET/MRI "remains to be seen," Hoffmann and colleagues added, since only a handful of studies have been published on this topic.
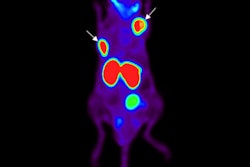
One such area of clinical efficacy is in the staging of lymph nodes, especially in the pelvis. A 2016 study by Maurer et al of 130 consecutive patients with intermediate- to high-risk prostate cancer found specificity of 99% and accuracy of 88% with Ga-68 PSMA PET, compared with 85% for CT alone and 72% for MRI alone -- prior to radical prostatectomy and pelvic lymph node dissection (Journal of Urology, May 2016, Vol. 195:5, pp. 1436-1443).
A 2017 prospective multicenter study by Roach et al showed that Ga-68 PSMA PET/CT results directly changed the management in 51% of 431 prostate cancer patients. Individuals with an indication of biochemical recurrence after surgery had a management change rate of 64%, while those who had received radiation therapy had a treatment change rate of 69%. In addition, patients who underwent scans for primary staging had a treatment change rate of 23%.
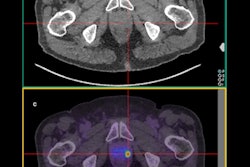
There is, however, one major drawback of Ga-68 PSMA and other PSMA-targeting PET tracers, the researchers noted. That is radiotracer accumulation in the urinary tract and bladder, which can cause a "halo" artifact effect and reduce the visibility of the tumor. Hoffmann and colleagues expect PET tracers now under development, such as F-18 PSMA-1007, should minimize this imaging obstacle "due to its substantially reduced urinary clearance," especially with PET/MRI scanners.
The researchers recommended additional studies and randomized trials to confirm Ga-68 PSMA's clinical value, such as assessing the long-term outcomes of patients with negative PSMA PET scans whom clinicians chose not to treat.