Cancer is now the leading cause of death in high-income countries, with twice as many people dying from cancer than heart disease in these nations. Heart disease continues to be the main cause of death in less prosperous countries, according to data presented at this week's European Society of Cardiology (ESC) meeting in Paris.
Two reports from the Prospective Urban and Rural Epidemiologic (PURE) study provide new information on common disease incidence, hospitalization, and death, as well as modifiable cardiovascular risk factors in middle-aged adults across 21 nations. The findings have also been published online on 3 September by the Lancet.
Cardiovascular disease remains the leading cause of mortality among middle-aged adults globally, accounting for 40% of all deaths, but this is no longer the case in more developed nations where cancer is now responsible for twice as many deaths as heart disease, according to lead author Dr. Gilles Dagenais, emeritus professor at Laval University in Quebec, Canada, and colleagues. They estimated that 55 million deaths occurred in the world in 2017, of which approximately 17.7 million were due to cardiovascular disease.
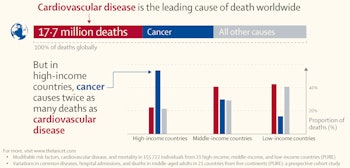
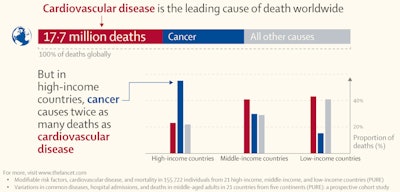
Cancer deaths versus cardiovascular disease deaths. Image courtesy of the Lancet.
Dagenais's group followed 162,534 middle-aged adults (ages 35-70, 58% women) in four high-income, 12 middle-income, and five low-income countries over a median of 9.5 years (between 2005 and 2016). They found that cardiovascular-related deaths were 2.5 times more common in middle-aged adults in poorer nations compared with richer countries, despite the former experiencing a substantially lower burden of cardiovascular risk factors compared with the latter.
"The world is witnessing a new epidemiologic transition among the different categories of noncommunicable diseases," noted Dagenais in a statement issued by the Lancet. "Our report found cancer to be the second most common cause of death globally in 2017, accounting for 26% of all deaths. But as cardiovascular disease rates continue to fall, cancer could likely become the leading cause of death worldwide within just a few decades."
The authors suggest that higher cardiovascular-related mortality in low-income countries may be largely due to lower quality of healthcare, given that the report found first hospitalization rates and cardiovascular disease medication use to both be substantially lower in low- and mid-income countries, compared with richer nations.
The study found the incidence of heart disease per 1,000 person years to be 7.1, 6.8, and 4.3 in low-income, middle-income, and high-income countries, respectively, but it also found cancer, pneumonia, chronic obstructive pulmonary disease, and injuries to be least common in low-income nations and most common in wealthier nations. Overall, mortality rates were twice as high in poorer countries compared with mid-income nations, and four times higher in poorer countries compared with high-income nations, though rates of deaths from cancer were similar across all country income levels.
Governments in poorer countries need to invest more of their gross domestic product in preventing and managing noncommunicable diseases rather than focusing mainly on infectious diseases, according to Dr. Salim Yusuf, professor of medicine at McMaster University in Hamilton, Canada, and principal investigator of the study.
Modifiable risk factors
A second report from the PURE study explored the relative contribution -- population attributable factor, or PAF -- of 14 modifiable risk factors to cardiovascular disease among 155,722 community-dwelling, middle-aged people without a prior history of heart disease, within the same 21 countries.
Overall, modifiable risk factors, including metabolic, behavioral, socioeconomic, and psychosocial factors, strength, and environment, accounted for 70% of all CVD cases globally. Metabolic risk factors were the largest contributory risk factor globally (41.2%), with hypertension (22.3%) the leading factor within this group.
However, the relative importance of risk factors for cases of cardiovascular disease and death varied widely between countries at different stages of economic development. For deaths, the largest group of PAFs overall were for behavioral risk factors (26.3%), but in mid- and low-income nations, the importance of household air pollution, poor diet, low education, and low grip strength were substantially larger compared with their impact in richer countries. Metabolic risk factors like high cholesterol, abdominal obesity, and diabetes played a larger role in causing heart disease in high-income nations.
"While some risk factors certainly have large global impacts, such as hypertension, tobacco, and low education, the impact of others, such as poor diet and household air pollution, vary largely by the economic level of countries," said Sumathy Rangarajan, program director at the Population Health Research Institute, McMaster University, who coordinated the study. "There is an opportunity now to realign global health policies and adapt them to different groups of countries based on the risk factors of greatest impact in each setting."
Efforts to tackle cardiovascular disease by focusing on a small number of behavioral risk factors, such as reducing smoking, are important, but these efforts should expand to better blood pressure control and better use of secondary prevention with simple and effective low-cost medications, added Dr. Philip Joseph, associate professor of medicine at the same institution.
Research limitations
Despite being the only research involving as many as 21 countries in a cohort study, caution should be exercised in generalizing results to all countries, the authors noted. In particular, PURE does not include data from West Africa, North Africa, or Australia. Also, the number of participants from the Middle East is modest, and data from low-income countries are predominantly from South Asia with a few African countries.
Despite these limitations, Stephanie Read, PhD, and Sarah Wild, PhD, both from the University of Edinburgh in the U.K., wrote in a linked comment, "[These] findings can inform the effective use of limited resources -- for example, by indicating the importance of improving education across the world and improving diet and reducing household air pollution in less developed countries. The value of collecting similar data to inform policy in a wider range of countries is clear, while improving lifestyle choices and modifying their social and commercial determinants remain a challenge."
The PURE study is the only large prospective international cohort study that involves substantial data from a large number of countries and employs standardized and concurrent methods of sampling, measurement, and follow-up, according to the Lancet. Countries analyzed in these two reports from the PURE Study include: Argentina, Bangladesh, Brazil, Canada, Chile, China, Colombia, India, Iran, Malaysia, Pakistan, Palestine, the Philippines, Poland, Saudi Arabia, South Africa, Sweden, Tanzania, Turkey, United Arab Emirates, and Zimbabwe.




















