Prostate cancer PET scans can help predict how long patients may survive disease-free after radical prostatectomy, according to a study published March 17 in the European Journal of Nuclear Medicine and Molecular Imaging.
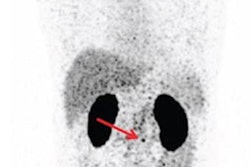
Australian researchers investigated whether the signal intensity of prostate-specific membrane antigen (PSMA) on gallium-68 (Ga-68) PET/CT scans was related to cancer recurrence after patients underwent radical prostatectomies. The findings suggest PSMA intensity is a novel, independent prognostic factor for biochemical recurrence, according to the authors.
"Our data provide strong clinical validation that high PSMA expression indicates aggressive disease," wrote lead author Dr. Matthew Roberts, a urologist at Royal Brisbane and Women's Hospital in Brisbane.
PSMA is a protein overexpressed by prostate cancer cells. Ga-68 PSMA is a radiotracer designed to bind to this protein and is used primarily to provide clinicians with information on whether prostate cancer has recurred after prostatectomies.
Preliminary evidence in small studies suggests Ga-68 PSMA-PET can also provide more prognostic data based on maximum standardized uptake values (SUVmax) of the Ga-68 PSMA tracer in primary tumors prior to surgery, according to the authors.
Further validation is required before Ga-68 PSMA values can be incorporated with other clinical variables to predict prostate cancer recurrence, they stated.
In this prospective analysis, the Australian group analyzed SUVmax levels in 848 men with prostate cancer who underwent radical prostatectomies at their hospital in Brisbane between August 2014 and June 2018.
Ga-68 PSMA PET/CT was most commonly performed in participants after prostate biopsy for staging purposes for surgery. Imaging was performed using either Ingenuity (Philips Healthcare) or Discovery MI (GE Healthcare) scanners, with SUVmax values reported by experienced nuclear physician radiologists, the authors wrote.
The primary outcome was biochemical recurrence-free survival in patients following radical prostatectomy or the beginning of radiotherapy or androgen deprivation therapy. Recurrence was defined as serum prostate-specific antigen (PSA) > 0.2 ng/ml.
The researchers found that primary tumors were PSMA-avid (SUVmax ≥ 3) in 92% of patients. The median SUVmax was 5.6 (interquartile range, 3.9-8.6).
After a median follow-up of 41 months, the researchers observed cancer recurrence in 155 men, while 64 commenced therapy. The estimated three-year biochemical recurrence-free survival rate for the group was 79% and the five-year recurrence-free rate was 70%, according to the findings.
Higher SUVmax was associated with shorter biochemical recurrence-free survival when analyzed as a continuous variable or by quartiles, the researchers noted. The three-year biochemical recurrence-free survival for SUVmax quartile four was 58%, compared with 91% for SUVmax quartile one.
In addition, in a Cox model adjusting for age and presurgical parameters, such as PSA, PI-RADS, and biopsy Gleason score, SUVmax was significantly associated with time to biochemical recurrence, with a hazard ratio of 1.15 per five-unit SUVmax increase, the authors reported.
"Clinicians can expect worse pathological and biochemical survival outcomes in patients with high primary tumor SUVmax values," the researchers wrote.
Current methods for estimating postoperative disease recurrence in patients who have undergone radical prostatectomies are limited in their accuracy, and incorporating novel imaging techniques can improve predictive tools, the authors wrote.
Ultimately, the findings in this study provide strong clinical validation that high PSMA expression detected on PET/CT indicates aggressive disease, independent of other clinical established factors, they wrote.
"We encourage further research to confirm these findings in relation to metastasis-free survival, as well as prospective trials using PSMA PET intensity to guide treatment decisions," Roberts and colleagues concluded.