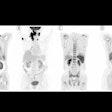
The U.S. Centers for Medicare and Medicaid Services (CMS) announced on October 13 that it has lifted its coverage limit of one beta-amyloid PET scan per lifetime for patients with Alzheimer’s disease.
The decision, which removes the previous national coverage determination and ends coverage with evidence development for beta-amyloid PET, comes in the wake of recent U.S. Food and Drug Administration (FDA) approvals of the first drugs to treat the disease – monoclonal antibodies that target brain amyloid plaque deposits. Medicare coverage decisions for amyloid PET scans will now be made by local Medicare Administrative Contractors (MACs).
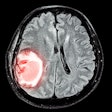
“Amyloid PET scans can be used to confirm evidence of brain amyloid pathology to select appropriate patients for proven anti-amyloid treatments depending on individual patient characteristics,” the CMS noted, in its decision memo.
Amyloid PET scans are a key diagnostic tool enabling clinicians to identify and confirm the presence of amyloid plaques – one of the hallmarks of the disease – in the brains of patients and thus ensure appropriate treatment.
While methods other than amyloid PET for identifying pathologic brain amyloid exist or may be emerging (cerebral spinal fluid analysis, which requires a lumbar puncture or simple blood tests), currently amyloid PET is the most-used method, the CMS noted.
The decision was applauded by national associations, many of which expressed support for the action during the comment period. In a statement, the Society of Nuclear Medicine and Molecular Imaging (SNMMI) said the decision will expand access for patients to a vital nuclear medicine test.
"This decision ensures increased accessibility to this crucial nuclear medicine test for eligible patients and facilitates the targeted use of new treatments for those who can benefit," said SNMMI president Helen Nadel, MD.
Ultimately, the CMS decision fell short of the hopes of most patient advocacy groups and national associations, which overwhelmingly asked the agency to reconsider leaving coverage determinations for the scans to the discretion of local Medicare Administrative Contractors (MACs) and instead implement a national coverage ruling.
In the final decision memorandum, the CMS wrote: “MACs also use an evidence-based process for making coverage determinations. Based on the evidence, we believe there will be consistent coverage across regions for appropriate Medicare patients.”
That statement is encouraging, noted the Medical Imaging and Technology Alliance (MITA).
“MITA calls on CMS and the MACs to work with neurology and Alzheimer’s disease stakeholders to ensure there is seamless and consistent coverage for amyloid PET,” MITA said, in a statement.
CMS initiated a reconsideration of its national coverage determination for amyloid PET in June 2022.