SAN ANTONIO - The first-ever study on the clinical use of PET/MRI and a breakthrough on the use of FDG-PET to detect fevers of unknown origin were among the top research papers outlined Monday at this week's Society of Nuclear Medicine (SNM) annual meeting.
More than 1,000 papers were submitted for consideration and presentation at this year's meeting, with many studies showing how molecular imaging is gaining influence in the early detection of Alzheimer's disease. Other submissions included a first-of-its-kind study on the use of near-infrared fluorescence and a new synthesized imaging agent to discover hidden blood clots in veins and arteries.
Hybrid PET/MRI
Early results from the clinical use of PET/MRI indicate that the hybrid modality can provide important diagnostic information about soft tissues and physiological functions throughout a patient's body. The technology's ability to find suspicious lesions and potential cancer already appears comparable to that of conventional molecular imaging methods.
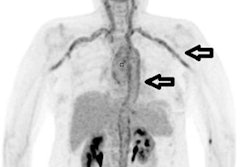
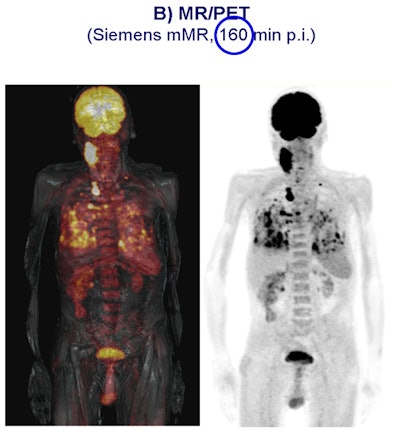
In a German study, 11 patients with cancer underwent single-injection PET/CT followed by PET/MRI (Biograph mMR, Siemens Healthcare). Simultaneous PET/MRI acquisition was feasible and offered good-quality PET and MRI diagnostic data.
The analysis found that all 13 lesions detected at PET/CT were also identified by PET/MRI, with no significant difference between PET/CT and PET/MRI regarding the uptake ratios.
The study "demonstrates for the first time that newly introduced integrated whole-body MR/PET technology allows simultaneous acquisition of high-quality MR and PET data in a clinical setting within an acceptable time frame," wrote lead study author Dr. Alexander Drzezga from TU München.
The hybrid technology could result in the development of new imaging agents that combine the diagnostic prowess of PET and MRI, Drzezga said. With the ability to image physiologic and pathophysiologic processes at the same time, the technology could open a new imaging discipline within nuclear medicine.
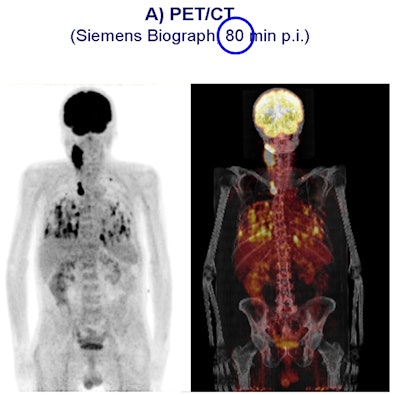 |
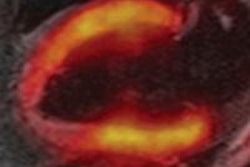
| Carcinoma is compared in a patient who received a PET/CT scan 80 minutes after contrast injection (above), followed by a PET/MRI scan 160 minutes after contrast injection (below). All images courtesy of SNM. |
 |
FDG-PET and fever of unknown origin
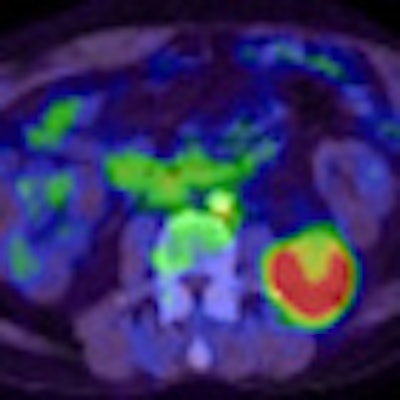
Japanese researchers broke new ground in their study, which concluded that FDG-PET provided additional diagnostic information in cases of fever of unknown origin. The use of FDG-PET also had a high clinical impact, especially among patients with infectious diseases.
The retrospective study evaluated 81 consecutive patients with fever of unknown origin. They underwent FDG-PET at six Japanese institutions between July 2006 and December 2007.
Results were divided into four groups for final diagnoses: infection, arthritis/vasculitis/autoimmune/collagen disease, tumor/granuloma, and other/unknown.
The analysis found that sensitivity was highest in the tumor/granuloma group at 100% (seven of seven cases), followed by infection at 89% (24 of 27 cases) and arthritis/vasculitis/autoimmune/collagen disease at 65% (11 of 17 cases). Sensitivity was 0% (zero of one case) in the other/unknown category. Overall sensitivity was 81% and overall specificity was 75%.
Additional information provided by FDG-PET was highest in the infection group, at 76% of the cases (22 of 29), followed by tumor/granuloma at 75% (six of eight), arthritis/vasculitis/autoimmune/collagen disease at 43% (nine of 21), and other/unknown at 23% (five of 22).
The other/unknown group showed a high specificity of 84% (16 of 19 cases) and accurately excluded active focal inflammatory diseases and malignancy.
Lead study author Dr. Kozuo Kubota, PhD, chief of nuclear medicine at the National Center for Global Health and Medicine in Tokyo, said that until now, conventional modalities have produced low imaging resolution and very poor detectability for the fever's cause.
"If the CT scan, ultrasound, or other conventional imaging technique fails, it is very difficult to find ways to find the focus of the fever," Kubota said. "If we use FDG-PET, we can scan from head to thigh in only one scan to detect where the truly active lesion is. FDG is very sensitive both for inflammation and the tumor."
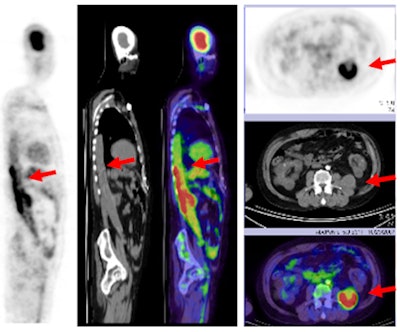 |
| With the addition of FDG-PET, physicians discovered a graft infection in a 50-year-old male with kidney failure and fever of unknown origin, with high FDG uptake illustrating the malady. |
"I view this [study] as extraordinary," said Dr. Michael Graham, PhD, director of nuclear medicine at the University of Iowa, who announced the top five papers. "This is in a setting where modern medicine is unable to come up with the answer, even after weeks. In about an hour-and-a-half, an FDG-PET scan came up with the answer with excellent sensitivity. We don't get it every single time, but if it weren't done, it would be mysterious what the patient had. It would be treated with antibiotics and hope for the best."
"This is a huge step forward and I think it will change how we approach this problem," he said.
PET and Alzheimer's detection
Three studies presented at SNM 2011 added to the growing evidence that PET is an effective method to detect Alzheimer's disease in its early stages, and that it provides a pathway to future clinical screening and treatments.
One lead study author, Dr. Kevin Ong, research scientist at Austin Hospital in Heidelberg, Australia, said that amyloid imaging with PET scans can help ascertain the likelihood that individuals will deteriorate cognitively within a few years, enabling more efficient channeling of healthcare resources.
Molecular imaging of Alzheimer's disease has focused on detecting and analyzing the formation of the protein beta amyloid in the brain, which researchers say is directly involved in the pathology of Alzheimer's. The presence of significant amyloid buildup is also linked to more rapid memory decline and brain atrophy.
Increased amyloid is bad for cognition even in the healthy elderly, noted lead study author Michael Devous Sr., PhD, director of neuroimaging for the Alzheimer's Disease Center at the University of Texas Southwestern Medical Center.
The three ongoing studies involve several years of research based on hundreds of participants ranging widely in age, cognitive ability, and stage of disease.
Collective results showed that amyloid plaques build up at an estimated rate of 2% to 3% per year, and they often are already present in healthy older individuals. Amyloid plaque was present in 12% of people in their 60s, 30% of those in their 70s, and 55% of those older than 80.
In one study, approximately 25% of subjects older than 60 had amyloid plaques.
For individuals who have already developed a measurable memory decline, a positive scan for amyloid is the most accurate predictor of progression to Alzheimer's disease, said Dr. Christopher Rowe, a lead investigator for the Australian Imaging, Biomarkers, and Lifestyle study of aging and professor of nuclear medicine at Austin Hospital.
Amyloid imaging with PET scans, he added, will be an important new tool in the assessment of cognitive decline.
Several studies have used carbon-11-labeled Pittsburgh Compound B (C-11 PIB), a PET imaging agent that binds to beta amyloid in brain tissue, but two of the current studies are assessing the benefit of F-18 florbetaben and F-18 florbetapir, which are designed for routine clinical use.
Both F-18 florbetaben and F-18 florbetapir are showing promise as reliable predictors of progression to Alzheimer's disease, and F-18 amyloid imaging agents are considered most likely to move into clinical practice in the near future, perhaps as soon as next year.
NIRF for blood clot detection
In another novel study at SNM 2011, researchers from Massachusetts General Hospital are using near-infrared fluorescence (NIRF) and a new synthesized imaging agent to detect blood clots inside elusive veins, often within the deep tissues of the thighs and pelvis.
The agent uses a biomarker that seeks out a peptide -- called fibrin -- that is actively involved in the formation of blood clots. Combined with NIRF, which uses light energy to gather information from cells and tissues, the technique could also be used for coronary arteries. The fibrin peptide agent (EP-2104R) has already been tested in phase II clinical trials.
Lead study author Dr. Tetsuya Hara, PhD, noted that the availability of a high-resolution fibrin sensor is important for two reasons: intravascular NIRF imaging of coronary-sized arteries is now possible, and coupling the fibrin peptide with this technique may allow researchers to study coronary artery plaques and stents, which could potentially help identify patients at increased risk of heart attack.
The researchers were able to successfully detect fibrin-rich deep vein thrombosis with both intravital fluorescence microscopy and noninvasive fluorescence molecular tomography, allowing information to be acquired about tissues by analyzing how light is absorbed and scattered.
By coupling the fibrin peptide agent with intravascular NIRF imaging, researchers can now study microthrombi on coronary artery plaques and coronary stents that are at high risk for thrombosis and vessel occlusion.
This advance could help clinicians predict potential heart attacks and other major cardiovascular events, potentially saving more patients' lives.