The seven-year initiative known as the National Oncologic PET Registry (NOPR) began to wind down its operation after the U.S. Centers for Medicare and Medicaid Services (CMS) announced last month it would halt the data collection requirement for all oncologic indications for FDG-PET as a condition of reimbursement.
NOPR is no longer accepting new cases for FDG-PET, but it will continue to collect information for sodium fluoride (NaF) PET imaging to accumulate evidence on its efficacy.
Since May 8, 2006, when NOPR opened, the program has gathered results on a coverage with evidence development (CED) basis of how FDG-PET influenced treatment strategies and patient outcomes for a variety of cancers, including brain, cervical, small cell lung, pancreatic, testicular, and ovarian.
The most significant breakthrough for the registry occurred in 2009, when CMS expanded coverage for nine cancers, along with the initial diagnosis and subsequent treatment strategy. The nine cancers were breast, cervical, colorectal, esophageal, head and neck, lymphoma, melanoma, non-small cell lung, and thyroid.
In addition, Medicare expanded coverage to ovarian cancer and myeloma, making a total of 11 indications covered for both the initial diagnosis and treatment.
"I believe that CMS is pleased with the way this came out, as it is probably its most successful CED program to date, certainly in terms of changing public policy in coverage," said NOPR co-chair Dr. Barry Siegel, professor of radiology and chief of the division of nuclear medicine at the Mallinckrodt Institute of Radiology at Washington University.
NOPR founders
Siegel has been with NOPR from the start, along with NOPR chairman Dr. Bruce Hillner from the department of internal medicine at Virginia Commonwealth University. NOPR lost its other co-chair, Dr. R. Edward Coleman, who passed away in June 2012. The world-renowned nuclear medicine specialist was the director of nuclear medicine and vice chairman of radiology at Duke University Medical Center.
 Dr. Barry Siegel from the Mallinckrodt Institute of Radiology.
Dr. Barry Siegel from the Mallinckrodt Institute of Radiology.
"I don't know if people have any idea how much effort, time, and work that [Drs. Siegel and Coleman] put into NOPR," said Kim Pierce, outgoing executive director of the World Molecular Imaging Society (WMIS). "It was an enormous amount of time, answering questions, calling people, and going over the data."
What may be most surprising is that NOPR handled the volume of incoming data from PET facilities around the U.S. with a rather small staff. Leading the effort was Siegel, Hillner, and, more recently, co-chair Dr. Anthony Shields, PhD, professor of medicine and oncology at Wayne State University.
In addition, there was Denise Merlino, coding advisor with the Society of Nuclear Medicine and Molecular Imaging (SNMMI), one person at the American College of Radiology office in Philadelphia to coordinate the entire project, and three statisticians at Brown University.
"All the data were collected electronically and went into a database, which the statisticians sliced and diced for us as necessary," Siegel said. "The people who really did the work were those at the individual PET facilities who were uploading the data."
Still, he added, NOPR provided a "relatively painless way" to get a PET scan for a patient who otherwise would not have received one. And even though much of the burden fell on referring physicians and PET facilities, the latter benefited from the additional patient volume and reimbursement.
NaF-PET registry
NOPR will continue to operate its NaF-PET registry; PET facilities need only continue sending their information to NOPR. PET facilities that currently participate but do not wish to continue should submit a request to CMS to withdraw from the program.
So far, the amount of data sent to the NaF-PET registry is far less than FDG-PET submissions. Siegel speculated that physicians in general are less familiar with NaF-PET imaging than with FDG-PET, and there is the additional burden of having to file the NOPR paperwork, which is not needed for a conventional bone scan. For non-Medicare patients, a conventional bone scan does not require precertification from a third-party payor, but NaF-PET imaging likely would require preapproval.
| NOPR registries | |||
| Opened | PET scans registered | Facilities with at least 1 PET scan |
|
| NOPR I | May 8, 2006 | 157,453 | 1,693 |
| NOPR II | April 6, 2009 | 175,841 | 1,871 |
| NaF-PET | February 7, 2011 | 20,238 | 852 |
"Because the marginal gain of sodium fluoride PET is not as widely perceived in the community as the marginal difference between an FDG-PET study and only doing CT, MRI, or other imaging, [NaF-PET] is taking off less rapidly," he added.
"I think sodium fluoride PET would shine for a variety of benign bone diseases, but these uses are not covered by CMS because we are limited to the detection of osseous metastatic disease," Siegel said. "How that coverage will evolve with CMS remains to be seen."
Siegel expects a study on the NaF-PET results to date to be finalized in the next few weeks and then submitted for publication. "Once we get that accepted, the goal likely will be to go back to CMS once again to ask for reconsideration," he said.
What's next?
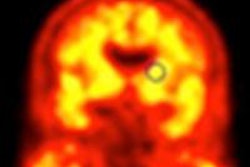
Beyond data collection for NaF-PET, NOPR's future is unknown. One possible use for the data-gathering infrastructure currently in place is to assess the efficacy of PET agents for detecting beta-amyloid deposits, which have been linked to cognitive impairment and Alzheimer's disease, Siegel said.
However, it may be a large step to go from PET imaging for oncology to beta-amyloid scans.
"If the study is put together with verifiable end points, it can be very helpful in gathering information," said Dr. Gary Dillehay, president of SNMMI and professor of radiology at Northwestern Memorial Hospital. "The benefit for the oncology patient is that you can find out within a year or two whether you are making a significant change in patient management or patient outcomes."
Conditions such as beta-amyloid accumulation or dementia, however, have a much longer time frame before results can be confirmed.
"If you have to wait until somebody dies, that may be 10 or 15 years, depending on their age and the time of [dementia] onset," Dillehay said. "We are not convinced that this particular method will work with dementia evaluation because the timeline is too long before you can confirm what you saw with an amyloid study."
NOPR's legacy
As for Siegel staying on board to navigate NOPR into the future, he said he is ready to turn the helm over to someone else, but he will continue to help guide the process.
"I don't know that I am necessarily going to be the one answering all the emails all day long, which I have been doing for the past seven years for FDG NOPR," he said.
In its wake, Siegel believes that NOPR's greatest accomplishment may be the PET community's improved relations with CMS.
"Probably the most important end product of NOPR is that the PET community went from having a predominantly adversarial and not terribly happy relationship with CMS to what I now consider to be a collaborative working relationship with CMS, seeking common goals to improve the health of Medicare beneficiaries," he said.
That sentiment was echoed by Pierce of WMIS.
"We ended up in a very positive relationship," she said. "All in all, we have come a long, long way. I think that if NOPR had not happened, we would still be [getting reimbursement for] one indication at a time."