CHICAGO - Adding diffusion-weighted imaging (DWI) to FDG-PET/MRI to stage women with primary or recurrent pelvic malignancies contributes minimal value and is not worth the additional scan time, according to a study from Germany presented on Sunday at RSNA 2014.
The study, presented by Dr. Johannes Grueneisen from the department of diagnostic and interventional radiology and neurology at University Hospital Essen, showed that omitting DWI from the whole-body PET/MRI protocol reduced scan time significantly and did not adversely affect diagnoses.
PET/MRI conundrum
Within the past decade, hybrid imaging, such as with PET/CT, has become a well-established tool in staging oncology patients. More recently, integrated PET/MRI has been used for a wide range of clinical applications, but "only a few studies have compared the staging performance between PET/CT and PET/MRI and reported more or less comparable results," Grueneisen told attendees.
Compared with PET/CT, PET/MRI provides "remarkably reduced radiation exposure and a high number of available MR sequences for certain issues," he added. "On the other hand, PET/MRI suffers from a markedly long examination time that potentially results in patient discomfort. So, using PET/MRI as a staging tool, there is a need for implementation of suitable MR protocols for certain tumor entities."
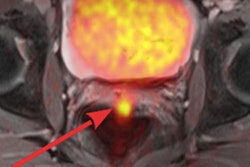
DWI, meanwhile, has been used effectively in cancer evaluation, as the MRI technique detects altered water diffusion in highly cellular tissue, such as malignant tumors.
The current study included 48 patients with a mean age of 53 years (± 12 years). Of the 48 women, 27 had primary pelvic disease and 21 had suspected pelvic tumor recurrence. All patients underwent a whole-body FDG-PET/MRI exam (Biograph mMR, Siemens Healthcare), which ranged from 40 to 45 minutes.
PET scans were done using four to five bed positions, depending on patient size. The whole-body MRI protocol included scans with and without DWI, with a focus on the female pelvis.
A total of 122 suspect lesions were discovered with the scans; 98 tumors were malignant and 24 were benign. The lesions were predominantly found in the lymph nodes (40 malignant and 18 benign) and in primary tumor sites (30 malignant and four benign); they were less prominent in the lung, bone, and liver.
Two radiologists separately evaluated the FDG-PET/MRI results without DWI, followed by a second reading with DWI. Their analysis included overall lesion detection, in which all lesions considered malignant were evaluated for lesion conspicuity on a four-point scale and diagnostic confidence was rated on a three-point ordinal scale.
In a second reading session, the pair qualitatively assessed lesion-to-background contrast and diagnostic confidence for PET and DWI.
Head-to-head comparisons
The lesion-based analysis found that FDG-PET/MRI with DWI detected 91 (92%) of 98 malignant lesions and 21 (87%) of 24 benign lesions. Without DWI, FDG-PET/MRI found 93 (94%) of the 98 malignant lesions and 20 (83%) of the 24 benign lesions.
FDG-PET/MRI with DWI had lesion conspicuity of 3.6 ± 0.8, compared with 3.8 ± 0.7 for PET/MRI without DWI. Diagnostic confidence was less for PET/MRI with DWI (2.5 ± 0.7) than without DWI (2.7 ± 0.6).
Based on the results, Grueneisen and colleagues concluded that DWI with FDG-PET/MRI does not result in significantly higher detection of malignant lesions, while PET provides better lesion conspicuity and diagnostic confidence than DWI.
"DWI in a PET/MR protocol does not provide diagnostic benefit for staging or restaging female patients with pelvic malignancies, which are known to be FDG-avid," Grueneisen added. "The omission of DWI may offer a distinctive reduction in scanner duration of 10 to 14 minutes, which would be accompanied by an improvement in patient comfort."
He did cite some limitations of the study. For example, the heterogeneous study population included primary and recurrent tumors. Also, because the researchers were unable to obtain histopathologic information for all lesions, they used a modified reference standard based on histopathologic confirmation or cross-sectional imaging information over six months.