The ability of FDG-PET/MRI to detail morphology and assess malignancy makes it a "powerful tool" for the diagnostic workup of cardiac tumors, but it should be used judiciously because of its high cost and limited availability, according to a new study from Germany in the February Journal of Nuclear Medicine.
Led by Dr. Felix Nensa from the department of diagnostic and interventional radiology and neuroradiology at University Hospital Essen, the study found that FDG-PET and MRI separately achieved sensitivity of 100% and specificity of 92% in determining tumor malignancy. When the two modalities were combined, both sensitivity and specificity reached 100% for diagnosing malignancy (JNM, February 2015, Vol. 56:2, pp. 255-260).
While these preliminary findings are encouraging, the researchers cited several previous studies in which less costly and more readily available imaging modalities, such as CT, MRI, and echocardiography, were as effective as PET/MRI for assessing cardiac malignancy. FDG-PET/CT has also been found to offer useful diagnostic information for determining malignancy and staging cardiac tumors.
PET/MRI's potential
Previous studies of pathology outside the heart have found that FDG-PET with MRI can provide "superior morphologic tumor characterization and visualization of tumor metabolism," Nensa and colleagues wrote. Thus, they chose to explore the hybrid modality for cardiac tumors, comparing it with the use of MRI and FDG-PET alone.
The researchers started with 20 patients in the prospective study; 16 patients had cardiac masses, which were found by echocardiography (12 cases) and CT (four cases) but could not be identified. The other four patients had cardiac sarcoma after surgical therapy. Two subjects were later excluded from the analysis: One had an incomplete PET/MRI exam due to claustrophobia, while the other's suspected tumor was found to be an artifact.
All scans were performed on an integrated whole-body PET/MRI system with a 3-tesla magnet (Biograph mMR, Siemens Healthcare) and lutetium oxyorthosilicate (LSO) PET detectors. The PET imaging protocol included intravenous administration of 199 MBq (± 58 MBq) of FDG. The PET/MRI scan began approximately 94 minutes (± 35 minutes) after FDG injection, with a cardiac PET scan of 61 minutes (± 7 minutes) in one bed position and 3D image reconstruction.
The MRI protocol included the following sequences (in the following order): axial 2D half-Fourier acquisition single-shot turbo spin-echo (HASTE), balanced steady-state free precession (cine SSFP), 2D turbo spin-echo T1-weighted, and 2D turbo-inversion recovery-magnitude T2-weighted with short inversion time.
Two board-certified radiologists with more than 10 years of experience in cardiac MRI and oncologic PET interpreted the results and found that the maximum standardized uptake value (SUVmax) in malignant lesions (13.2 ± 6.2) was significantly higher than in nonmalignant cases (2.3 ± 1.2).
Tumor differentiation
A threshold of 5.2 or greater SUVmax resulted in 100% sensitivity and 92% specificity for differentiating malignant from nonmalignant lesions.
In addition, T2-weighted MRI with contrast enhancement yielded 100% sensitivity but only 46% specificity. Morphologic tumor features with cine MRI reached a sensitivity of 86% and specificity of 92%. Readers' interpretations using all MRI features yielded sensitivity of 100% and specificity of 92%.
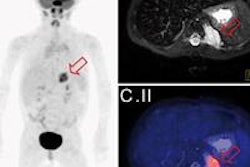
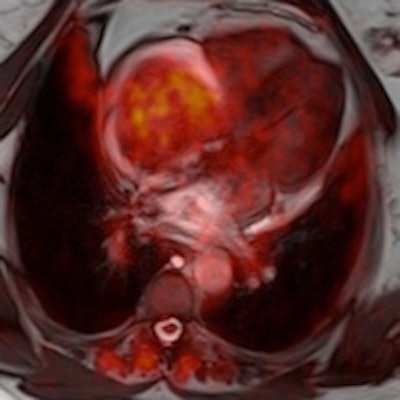
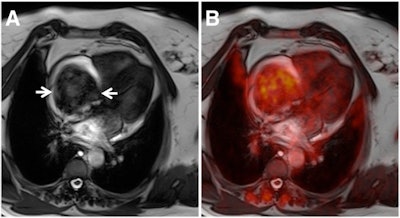 SSFP MR image (A) shows large intracavitary tumor in right atrium (arrows), causing dyspnea and thoracic pain. The fused PET image (B) illustrates mediocre FDG uptake in the tumor (SUVmax of 3.8). Histopathology confirmed the PET/MRI diagnosis of myxoma. Images courtesy of JNM.
SSFP MR image (A) shows large intracavitary tumor in right atrium (arrows), causing dyspnea and thoracic pain. The fused PET image (B) illustrates mediocre FDG uptake in the tumor (SUVmax of 3.8). Histopathology confirmed the PET/MRI diagnosis of myxoma. Images courtesy of JNM.The researchers also found that all malignant tumors expressed contrast enhancement with T1-weighted MR images after injection of a gadolinium-based contrast agent. However, contrast enhancement was also found in seven (53%) of 13 nonmalignant cases.
Six (86%) of the seven malignancies were identified correctly by morphologic features using cine SSFP imaging, compared with 12 (92%) of 13 of correctly identified nonmalignant cases.
The authors concluded that independently interpreted FDG-PET and MRI results produced sensitivity of 100% and specificity of 92% in determining tumor malignancy. A combination of FDG-PET and MRI achieved 100% sensitivity and 100% specificity, when both tests were required to be positive for diagnosing malignancy.
Based on the results, Nensa and colleagues concluded that FDG-PET/MRI is a "powerful tool" in the diagnostic workup of cardiac tumors -- with caveats.
"Given the already strong performance of competitive methods such as PET/CT and MR imaging, high cost, and limited availability of PET/MR scanners, simultaneous PET/MR imaging might be reserved for selected cases for which true benefit can be expected," they wrote.
They also cautioned that the pilot study findings are preliminary and additional multicenter research is needed to confirm FDG-PET/MRI's efficacy in cardiac tumor assessment.