Selectively increasing radiotherapy dose in tumor areas with significant uptake of the PET radiotracer F-18 fluoromisonidazole (FMISO) does not necessarily improve outcomes for non-small cell lung cancer (NSCLC) patients, according to a phase II study published in the July issue of the Journal of Nuclear Medicine.
The study was conducted by 15 academic PET facilities across France. The researchers evaluated 54 patients with localized, advanced non-small cell cancers who were undergoing chemoradiotherapy.
All patients underwent two FDG-PET/CT and two FMISO-PET/CT scans on the same scanner and under identical conditions. In 24 (70%) of 34 patients who had positive FMISO results, the radiotherapy dose was increased up to 86 Gy on hypoxic areas identified on FMISO-PET/CT. However, this additional dose did not improve patient outcomes (JNM, July 2017, Vol. 58:7, pp. 1045-1053).
At the three-month follow-up, 31 patients (57%) showed a favorable response to the radiotherapy, including 17 (50%) of the 34 patients in the FMISO-positive group. At one year, overall survival was 63%, and disease-free survival was significantly longer among patients whose FMISO scans were negative (p = 0.004). Radiotherapy dose, however, was not associated with disease-free survival when adjusted for patients' FMISO status.
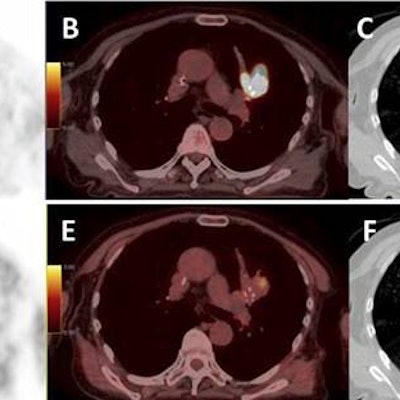
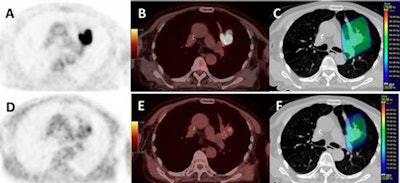 Images from a patient with an upper left lung NSCLC. (A) FDG; (B) FDG-PET/CT; (C) planning radiotherapy based on FDG (66 Gy) with BTVm (gross tumor volume), clinical target volume, and planning target volume; (D) FMISO-PET; (E) FMISO-PET/CT; and (F) boost based on the FMISO-PET (76 Gy) with BTVh (biological hypoxic target volume) and planning target volume boost. Images courtesy of Vera et al and JNM.
Images from a patient with an upper left lung NSCLC. (A) FDG; (B) FDG-PET/CT; (C) planning radiotherapy based on FDG (66 Gy) with BTVm (gross tumor volume), clinical target volume, and planning target volume; (D) FMISO-PET; (E) FMISO-PET/CT; and (F) boost based on the FMISO-PET (76 Gy) with BTVh (biological hypoxic target volume) and planning target volume boost. Images courtesy of Vera et al and JNM."Our approach results in a response rate of 40% or more with acceptable toxicity," concluded the group led by Dr. Pierre Vera, PhD, of the Henri Becquerel Cancer Center and Rouen University Hospital. "F-18 FMISO uptake in NSCLC patients is strongly associated with poor prognosis features that could not be reversed by radiotherapy doses up to 86 Gy."
On the positive side, the researchers noted that their approach of boosting radiotherapy based on hypoxia PET is feasible in a multicenter setting. The data also showed that smaller target volumes, identified by their functional characteristics using hypoxia PET/CT, can be adequately targeted. Finally, no significant toxicity has been associated with the radiotherapy boost.
In an invited perspective, also published in the July JNM, Dr. Rodney Hicks from the Peter MacCallum Cancer Centre and the University of Melbourne noted that negative results are instructive.
"Clearly, hypoxia remains an evil foe in our battle to achieve better outcomes in non-small cell cancer," he wrote. "But by demonstrating its importance, Vera and colleagues pose us the challenge to design new combination therapies."