German researchers found that mammography screening with a photon-counting digital mammography system turned in higher cancer detection rates at lower radiation doses than conventional digital mammography units in a real-world screening environment, according to a new study in Radiology.
The researchers examined cancer detection rates, recall rates, radiation dose, and other parameters for the photon-counting system, which they compared with other types of digital mammography units employed for screening in the state of North Rhine-Westphalia in Germany. Nearly 1 million women in total were screened in the study -- some 13,000 of whom received photon-counting mammography -- providing an ample population to assess the technology.
The only real drawback to photon-counting mammography was its recall rate, which was at least two percentage points higher than that of the conventional digital units. Study results from the research team, led by first author Dr. Stefanie Weigel and senior author Dr. Walter Heindel of University Hospital Muenster, were published online February 4 in Radiology.
New technology
Photon-counting mammography is one of the newer forms of x-ray-based mammography technologies. It's a variation on conventional digital radiography (DR) technology, in which a stationary tube delivers x-ray photons to a motionless digital detector.
 Dr. Walter Heindel.
Dr. Walter Heindel.
Photon-counting systems employ a slot-scanning design in which the system performs a lateral scan of the breast with a slot collimator. The unit's digital detector consists of an array of parallel silicon strips in combination with photon-counting electronics. The design reduces scatter radiation and noise and enables dose reduction, according to Weigel and colleagues.
Photon-counting mammography was initially developed by Swedish PACS firm Sectra, but the company sold the business in 2011 to Philips Healthcare. Sales of photon-counting mammography systems have been underway in Europe for years; Philips launched the technology in the U.S. in 2012, and it received clearance in February 2013 for the latest generation of the technology, MicroDose SI.
Previous research has found that photon-counting digital mammography delivers the lowest mean glandular dose, compared with conventional DR and computed radiography (CR) mammography, the authors noted. Smaller studies have found that photon-counting DR is not inferior to conventional DR mammography, and an Irish study with a larger patient population found it to be comparable to DR, but a limited number of performance parameters were included.
Therefore, the researchers sought to analyze photon-counting mammography in a large screening population, assessing its performance in areas such as cancer detection rate, recall rate, detection rate of ductal carcinoma in situ (DCIS), and radiation dose.
Large screening population
Weigel and colleagues drew their patient population from women examined as part of North Rhine-Westphalia's breast screening program from January 2009 to December 2010. This resulted in a total population of 1,007,134 women, of whom 13,312 were examined with a single MicroDose Mammography L30 system manufactured by Sectra. The rest of the women received a mix of conventional DR- and CR-based mammography.
In analyzing the data, the researchers found that the photon-counting unit compared favorably with the other digital mammography systems across a variety of parameters. Photon-counting mammography produced a breast cancer detection rate for the first screening exam of 1.07%, compared with 0.84% for conventional digital mammography. The technology's detection rate for subsequent screening rounds was 0.76%, compared with 0.59% for conventional technology (p = 0.05).
What's more, the higher cancer detection rate for photon-counting mammography came with lower radiation dose. Photon-counting mammography's mean glandular dose for craniocaudal views was 0.60 mGy ± 0.2, compared with 1.67 mGy ± 0.47 for conventional DR mammography. For mediolateral views, photon-counting mammography also had an advantage, with a mean glandular dose of 0.64 mGy ± 0.23, compared with 1.79 mGy ± 0.53 for conventional mammography (both p = 0.001).
On the downside, photon-counting mammography recorded a higher recall rate than that experienced in the rest of the screening program in North Rhine-Westphalia. Its recall rate for initial screening was 10%, compared with 7.6% for conventional DR mammography (p = 0.001), and 5.4% versus 3.4% for subsequent screening (p = 0.001).
Photon-counting mammography also showed a higher rate of DCIS detection than conventional digital mammography, at 0.23% versus 0.12% (p < 0.05), and a higher proportion of DCIS compared to all screening-detected malignancies, at 29.2% versus 20.7% (p = 0.01).
The findings echo previous studies that found an increase in the detection of microcalcifications with photon-counting mammography and, thus, higher rates of DCIS detection. The authors posited that the higher spatial resolution of photon-counting mammography, with a pixel pitch of 50 microns versus 70 microns for DR-based conventional mammography, could account for the difference, as DCIS tends to be depicted by calcifications.
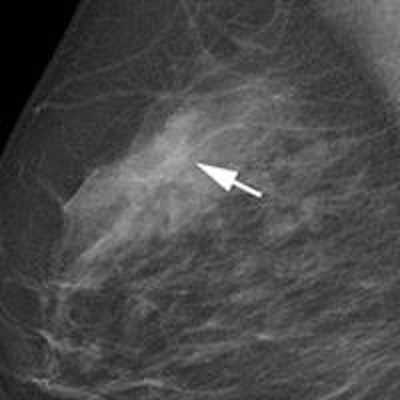
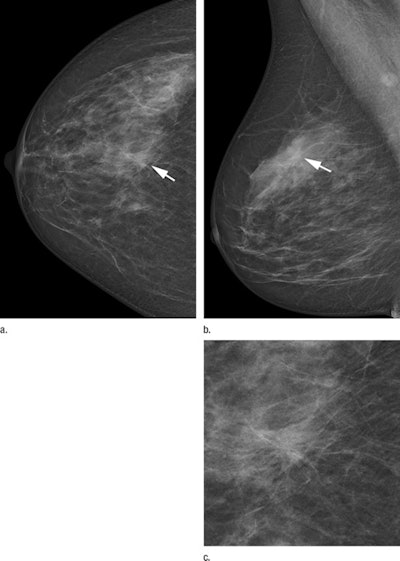 Two-view screening mammograms obtained with the DR photon-counting system show a spiculated mass in the right upper quadrants (arrow). The diagnosis was invasive ductal carcinoma, 8 mm in diameter, as seen on the (a) right craniocaudal image, (b) right mediolateral oblique image, and (c) zoomed in craniocaudal image of the lesion. Images courtesy of RSNA.
Two-view screening mammograms obtained with the DR photon-counting system show a spiculated mass in the right upper quadrants (arrow). The diagnosis was invasive ductal carcinoma, 8 mm in diameter, as seen on the (a) right craniocaudal image, (b) right mediolateral oblique image, and (c) zoomed in craniocaudal image of the lesion. Images courtesy of RSNA.Exceeding guidelines
The study shows that photon-counting mammography is suitable for sensitive breast cancer detection as measured by several key performance indicators, but this is balanced by the technology's higher recall rate, Weigel and colleagues noted when discussing the results.
"Our study showed that digital mammography screening by using the dose-efficient photon-counting technique enables detection of small invasive cancers and DCIS above the desirable level of the European guidelines," the authors wrote. "Higher cancer detection rates of invasive cancers and DCIS compared with other screening areas of the state were reached for subsequent screening at a higher recall rate."
Among the limitations of the study is that it was based on data from only one photon-counting mammography unit; also, the three readers were not blinded to the technique when interpreting images. As a result, the researchers couldn't distinguish whether the high recall rates were due to technique or reader factors.
Regarding future research, one topic could be investigating spectral imaging techniques with the system to quantify breast glandular tissue, which would address the confounding nature of breast density on mammography exams, according to the authors. The recently cleared MicroDose SI unit includes a special mode for spectral breast imaging.



















