Using computer-aided detection (CAD) with digital mammography has no significant effect on radiologists' performance when they interpret screening mammograms, and it doesn't change their diagnostic decisions, according to a new study published in the October issue of the American Journal of Roentgenology.
The study results add to the mixed opinions about the technology's benefits, wrote researchers from the Medical University of South Carolina.
"Although there was room for improvement in our radiologists' interpretations without CAD, few readers showed improved sensitivity after the application of CAD to digital mammograms," wrote lead author Elodia Cole and colleagues. "The readers in the present study rarely changed their diagnostic decision after the addition of CAD."
Mixed reviews
CAD for film-screen mammograms was introduced in the late 1990s, and ever since the technology began to be used clinically, radiologists have expressed concern that it produces high numbers of false positives, which can lengthen interpretation time, according to Cole's team (AJR, October 2014, Vol. 203:4, pp. 909-916).
"Each region of interest marked by CAD has to be looked at a second time by the radiologist, so even 0.5 false-positive marks per image (i.e., two false-positive marks per four-view mammogram) leads to an increase in interpretation time," the group wrote.
 Elodia Cole from the Medical University of South Carolina.
Elodia Cole from the Medical University of South Carolina.For this study, Cole and colleagues wanted to assess the impact of CAD on radiologist performance with digital mammograms acquired during the American College of Radiology Imaging Network's Digital Mammographic Imaging Screening Trial (DMIST). CAD was not used in DMIST; however, the researchers believed that DMIST offered a large database of digital mammography studies to which CAD could be applied retroactively.
"Concerns about high false-positive rates affecting study results, the limited clinical use of the technology, the lack of availability of the technology for digital mammography at that time, and the limited interest in CAD by radiologists on the DMIST trial design team are among the reasons why CAD was not used in DMIST," Cole and colleagues wrote.
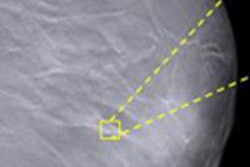
The researchers used DMIST cases proved to be cancer that had digital images. Fourteen radiologists interpreted a set of 300 cases (half with cancer, half benign) both with and without the help of CAD, using iCAD's SecondLook software; another 15 radiologists interpreted a different set of 300 cases (half malignant, half benign) using Hologic's R2 ImageChecker Cenova.
Each radiologist reader identified the presence of suspicious lesions, whether a recall was necessary, and the probability of malignancy using DMIST's seven-point scale for each exam, first without CAD and then with the technology. The researchers then assessed performance indicators such as sensitivity, specificity, and area under the curve (AUC) for each individual radiologist and the group as a whole.
For the entire group, overall sensitivity of the iCAD system for cancer cases included in the study was 0.75, while sensitivity of the R2 system was 0.73, Cole's team wrote. Overall false-positive detection rates for the two systems were 0.79 and 0.77, respectively.
While there were slight differences in group performance based on whether the radiologists did or did not use CAD, none of the differences were statistically significant, the researchers found.
| CAD's effect on radiologist performance | |||||
| Average AUC | Average sensitivity | Average specificity | |||
| iCAD readers | |||||
| Without CAD | 0.71 | 0.49 | 0.89 | ||
| With CAD | 0.72 | 0.51 | 0.87 | ||
| R2 readers | |||||
| Without CAD | 0.71 | 0.51 | 0.87 | ||
| With CAD | 0.72 | 0.53 | 0.86 | ||
In addition, CAD's input did not influence radiologist readers to change their cancer rating for 97.6% of the cases assessed using the iCAD software, and 98% of the cases assessed using the Hologic system, they wrote.
So what's it good for?
While CAD didn't seem to have an effect when the radiologists were assessed as a group, there were statistically significant differences when individual performances were analyzed: Four of the 14 iCAD readers and four of the 15 R2 readers did have improved AUC and sensitivity when they used CAD, Cole and colleagues found.
Why? Previous studies have hypothesized that CAD helps radiologists who have less mammography experience. However, this study did not find that correlation, which suggests that CAD's benefits interact with individual radiologists' skills -- or level of distraction, Cole said.
"We did not find correlation between those radiologists with less mammography experience and increased AUC and sensitivity rates with CAD," Cole told AuntMinnie.com. "But the purpose of CAD is to offer a second look, and there are radiologists in practice who may need it more than others."