CHICAGO -- Using AI to measure epicardial adipose tissue volume on routine low-dose CT (LDCT) imaging helps assess patients' risk of heart disease, according to research presented December 2 at the RSNA meeting.
Evaluating epicardial adipose tissue volume in this way appears to be effective beyond traditional clinical variables and coronary artery calcium (CAC) scoring, reported presenter Jong Eun Lee, MD, PhD, of Asan Medical Center in Seoul, South Korea.
"Incorporating [epicardial adipose tissue] assessment into health screening protocols could identify asymptomatic individuals who might benefit from preventive interventions, improving patient outcomes and clinical decision-making," he told session attendees.
Although the quantification of epicardial adipose tissue volume has traditionally been time-consuming, recent developments in AI have made rapid and reproducible measurements possible, Lee said. But the prognostic value of measuring epicardial fat in the setting of screening LDCT is unclear.
The investigators conducted a study that included 5,342 individuals aged 40 years or older asymptomatic for cardiovascular disease, who underwent LDCT between 2007 and 2014. They used a commercially available AI software (ClariCardio) to assess epicardial adipose tissue volume and mean attenuation (threshold, -190 to -30 Hounsfield units [HU]) and CAC score (threshold, 130 HU to Agatston score). The median follow-up period for major adverse cardiovascular events (MACE) was 7.5 years; during that time, there were 383 of these (7.2%). Finally, the team used the Net Reclassification Index (NRI) to assess improvements in risk stratification and cost-effectiveness.
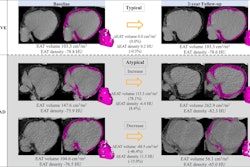
Overall, Lee reported that, after adjusting for AI-based CAC and clinical variables (age, sex, smoking status, hypertension, diabetes, obesity, lab findings), increased AI-based epicardial adipose tissue volume was significantly associated with a higher risk of a MACE, whereas epicardial adipose tissue density was not. He and his colleagues also found that the addition of AI-based epicardial adipose tissue volume to a model containing clinical variables and CAC significantly improved risk prediction (p = 0.048).
"[We found that] high and low epicardial adipose tissue volume provided additional stratification for MACE risk beyond the presence or absence of CAC," Lee said, noting two cases that demonstrated this result: a patient with a CAC score of 0 but with high epicardial adipose tissue volume who experienced a MACE during the follow-up period, and another with a low epicardial adipose tissue volume and a CAC score of 0 who did not.
"In an asymptomatic screening population undergoing LDCT, epicardial adipose tissue volume served as an independent prognostic factor beyond CAC, demonstrating improvement in future MACE prediction and risk reclassification," he concluded.
Visit our RADCast for full coverage of RSNA 2025.