Infection/Inflammation
Osteomyelitis
See section on "Infection"
Chronic recurrent Multifocal Osteomyelitis:
Despite its name, recurrent multifocal osteomyelitis is a rare idiopathic inflammatory condition in which the osseous findings mimic that of osteomyelitis, but no pathogens can be isolated from the involved areas (i.e.- non-bacterial or aseptic osteomyelitis) [9,10]. The disorder typically has a benign, self-limited clinical course with periodic exacerbations and remissions. Bone biopsy is mandatory for the diagnosis and demonstrates extensive fibrosis and inflammatory cells, but is culture negative. Patients usually present in late childhood or early adolescence (generally ages 9-14 years) with a single, locally painful, tender and swollen site- most commonly in the tibia. Onset can be insidious with variable duration of symptoms [9]. There is a slight female predominance (2:1) [9]. Systemic manifestations such as fever, weight loss, and lethargy are unusual, but can be seen [9]. ESR and C-reactive protein are typically mildly elevated with a normal WBC count [9]. Common sites of involvement are the long tubular bones (lower extremity three times more common than upper extremity- and most commonly the tibia) and the clavicles [9]. The lesions are located in the metaphysis (or metaphyseal equivalent) in 75% of lesions [9]. Complications can include premature physeal fusion and growth disturbances. The disorder has been associated with a rare cutaneous disorder known as palmoplantar pustulosis [9]. It has also been described in association with other inflammatory disorders such as psoriasis, Takayasu arteritis, Wegeners, Crohns disease and ulcerative colitis [9]. Antibiotics have no impact on the course of the disease which usually resolves spontaneously with time, although the disease course can be unpredictable (months to years) [9]. Symptomatic relief can be provided with non-steroidal anti-inflammatory agents.
On plain film, in the early stages, there are round or column-shaped osteolytic lesions located adjacent to the growth plate in the metaphysis [9]. With time, there is progressive sclerosis around the lytic lesion and development of periosteal reaction and hyperostosis [9]. Multiple metaphyseal lesions can be present at one site [9]. There is also characteristic involvement of the medial third of the clavicle- up to 30% of all CRMO lesions are located in the clavicle [9]. On plain film, there is sclerotic expansion of the medial portion of the clavicle [9]. The mandible is involved in about 5% of cases [9]. The spine is involved in only 3% of lesions- most commonly the thoracic spine [9]. MR is superior to plain film for the detection of sites of osseous involvement [10]. In one study, plain films were positive in only 16% of sites identified by MR imaging [10].
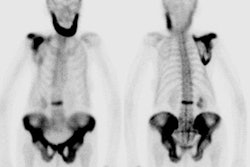
On scintigraphy, multifocal symmetric areas of increased tracer accumulation can be seen in up to two-thirds of cases. [2]
SAPHO syndrome:
Synovitis, acne, pustulosis, hyperostosis, and osteitis syndrome
(SAPHO) describes an association of sterile osteoarticular
inflammation with skin abnormalities- primarily palmoplantar
pustulosis and severe acne [12]. It is an inflammatory
spondyloathropathy and is the adult
equivalent of CRMO [9,11]. SAPHO syndrome is thought to result
from an exxaggerated immune response in geneetically susceptible
individuals to Propionibactrium acnes (an anaerobe
typically found in acne lesions) [12]. Patients present with pain,
swelling, and limitation of movement, most often in the anterior
chest wall, accompanied by fever and an elevated ESR and
C-reactive protein level [12]. The mean age of onset is 28
years and the prevalence of skin lesions such as palmoplantar
pustulosis is much higher [9]. More than half of patients exhibit
palmoplantar pustulosis which manifests as yellowish pustules and
vesicles limited to the palms and soles [12].
The radiographic manifestations of SAPHO
consist of hyperostosis and osteitis [11]. Unlike CRMO, chest wall
(sternoclavicular joint hyperostosis) and pelvic disease (SI
joint)
predominate in SAPHO [9]. Inflammatory costoclavicular
enthesopathy and small hyperostotic foci at the sternal end of the
first ribs are considered diagnostic [12]. The cortical
inflammation of SAPHO causes hyperostosis which manifests as
cortical and periosteal thickening and the medullaryb inflammation
causes osteitis which manifests as trabecular changes [12]. In
over 90% of patients, the lesions are accompanied at some point by
an adjacent inflammatory arthritis, including enthesitis and
anklyosis [12]. Also- adults with SAPHO can have arthritis of
peripheral joints and ossification of ligaments and entheses
(features
not typically seen with CRMO) [9]. Spinal invovlement is usually
monovertebral and may include spondylodiskitis (mimicking
infection), sclerosis, and expansion (mimicking Pagets disease),
asymmetric bulky paravetebral ossificiation and sacroiliitis
(mimicking psoriatic arthritis), and osteolysis including collapse
[12]. Vertebral body corner erosions are
consistently seen on MR in patients with SAPHO and may enhance
[11].
Signal abnormalities in contiguous vertebral bodies, narrowing of
disk
spaces, and pre-vertebral soft tissue enhancement can also be
present
and mimic diskitis or infection [11].
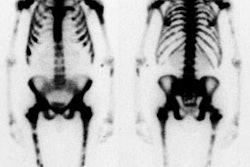
Bone scan will demonstrate prominent tracer uptake in the
sternclavicular regions producing a characteristic "bulls head"
sign [12].
Cultures are negative for
infection or may isolate low virulence organisms such as Propionibacterium acnes [11].
Treatment options include nonsteroidal antiinflammatory drugs,
corticosteroids, methotrexate, and tumor necrosis factor alpha
inhibitors [11]. The IV administration of second generation
bisphosphonates (such as pamidronate) may also be effective [11].
Septic Arthritis
Although septic arthritis can occur at any age, it is more common in young children (up to age 2), or adults with underlying joint disease. Monoarticular involvement is the most common pattern (90%). The most commonly involved joint is the hip in children, and the knee in adults. The most common organism is S. aureus. In children, other organisms encountered include: beta-hemolytic strep., gram negative bacteria, and H. influenzae type B (particularly in children less than 12 months old). Clinical findings include fever, pain, swelling, and erythema of the involved joint. In children, the affected hip is flexed, abducted, and laterally rotated (this position permits the largest volume of fluid in the joint). Rapid cartilaginous destruction can ensue and fibrous or bony ankylosis can eventually occur. Other complications include avascular necrosis (which may be related to local septic embolization and vascular compression by effusion), early osteoarthritis (due to cartilaginous destruction), and spread of the infection to the subjacent bone (osteomyelitis). Prompt drainage and antibiotic treatment is essential to prevent cartilage loss and other complications. Etiologies include hematogenous spread, direct inoculation from penetrating injury, or contiguous spread from an adjacent osteomyelitis. This latter etiology is frequently seen in infants under 18 months of age due to the presence of trans-physeal vessels which permit extension of a metaphyseal osteomyelitis to the epiphysis. Spread to the joint then occurs due to a shared blood supply by the epiphysis and the synovium.
The differential for septic arthritis includes transient synovitis which is commonly seen in children less than 10 years old, and characteristically follows a preceding viral URI. A joint effusion is commonly seen and usually resolves within a few days. Varying scintigraphic patterns have been associated with transient synovitis ranging from normal (most common) to 3-phase increased activity.
Early plain film evaluation of septic arthritis of the hip may demonstrate the presence of a joint effusion with joint space widening (greater than 2 mm difference from side to side), superolateral subluxation of the femoral head, or displacement of the capsular fat pads. Demineralization can be seen due to the associated hyperemia, or the presence of a metaphyseal osteomyelitis. Later, there is joint space loss followed by osseous destruction.
On 3-phase bone scan the inflamed joint demonstrates diffusely increased flow and blood pool activity. Delayed images generally demonstrate increased activity within the bone on either side of the joint. Differentiation from cellulitis may be difficult, but in cellulitis the underlying bone typically demonstrates only a mild increase in tracer activity. Septic arthritis is also suggested if the abnormality on bone scan is clearly synovial in distribution. Occasionally, decreased tracer uptake on delayed images may be seen in the femoral capital epiphysis as a result of vascular compression by the joint effusion. Once the elevated intraarticular pressure is relieved by arthrocentesis, uptake should return to the femoral head [1].
On MRI, up to 60% of cases of uncomplicated septic joint were associated with marrow signal changes that can be mistaken for osteomyelitis.
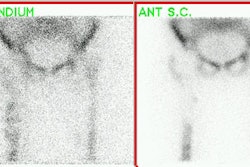
Necrotizing (Malignant) External Otitis:
NEO is a fulminant Pseudomonas infection of the external auditory canal complicated by local penetration into the underlying cartilage and subsequently the temporal bone which can result in osteomyelitis. The condition mainly affects diabetic patients [6]. Topical treatment is ineffective in these cases, and aggressive therapy with prolonged administration of systemic antibiotics and possibly local surgical debridment is required [6]. Clinically confirmed cases of malignant external otitis typically demonstrate no findings on plain film radiographs or CT imaging early in the course of the disease [7]. SPECT imaging is essential as it helps to separate bone involvement from adjacent soft tissue activity. Delayed (24 hours) images are also useful due to poor soft tissue clearance typically seen in diabetic patients. Lesion to non-lesion count ratios at 4 and 24 hours utilizing SPECT imaging can help in differentiating NEO from a severe external otitis. Although Ga-67 and In-111 WBC's are more sensitive in the detection of infection, they cannot differentiate between bone and soft tissue involvement. After making the diagnosis of NEO, however, Ga-67 scanning or In-111 WBC's can be used to follow the course of the infection as bone scans will often remain positive for prolonged periods of time despite effective treatment [4,6]. Upon successful treatment, Ga67 exams will normalize [7].
|
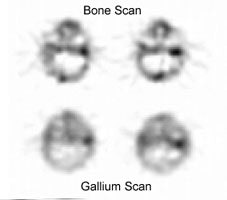
Malignant external otitis: Transaxial SPECT images from a Tc99m-MDP bone scan and a Ga67 scan demonstrate markedly asymmetric tracer accumulation within the left temporal bone in this patient with malignant external otitis. Gallium uptake ratios can be determined using the lesion to non-lesion side and these can be used to monitor response to therapy. |
|
|
Inflammatory Conditions:
Plantar Fasciitis:
Plantar fasciitis is a very common cause of heal pain and about one-third of the cases are bilateral [8]. The diagnosis is impiric and based on a history of heal pain that is worse in the morning and point tenderness over the anteromedial aspect of the inferior calcaneus [8]. Corticosteroid or local anesthesia injections is one method use to treat the condition [8]. In general, the condition is self-limiting with spontaneous resolution within 12 months in about 80% of patients, regardless of type of treatment [8].On bone scan, there is increased activity along the plantar aponeurosis on blood pool imaging and focal activity seen at the calcaneal insertion of the plantar aponeurosis on delayed images [8]. Focal hyperemia over the calcaneal insertion of the plantar aponeurosis on blood pool imaging seems to be associated with a higher success rate for corticosteroid injection [8]. More extensive abnormalities on blood pool imaging are associated with a decreased rate of success [8].
Sacroiliitis:
The diagnosis of sacroiliitis is often very subjective. Sacroiliitis, particularly if bilateral and relatively symmetric, can be difficult to detect due to the normal increased activity within the SI joints. Some authors feel that a SI joint to sacrum ratio of greater than 1.35 is abnormal, but others feel that quantitative indices are not reliable in differentiating normal from abnormal activity within the SI joints.
Synovial Inflammatory Disorders:
Both joint scanning (using Tc-pertechnetate) and blood pool images obtained with Tc-MDP will demonstrate increased tracer activity at sites of synovial inflammation. Gallium and In-111 WBC's will also accumulate at these sites. Differentiation of a septic arthritis from a non-infectious synovial inflammation is not possible by scintigraphy. Aspiration of the joint with culture of the synovial fluid is the best method for diagnosis.
Bone scan is also of limited value in the evaluation of juvenile rheumatoid arthritis. The prominent uptake of tracer within the growth plates often obscures increased periarticular tracer uptake, especially in small joints. In the knee, the lateral view may help to demonstrate increased activity in the patella as it projects free from the growth plate in this view.
REFERENCES:
(1) J Nucl Med 1998; Connolly LP, et al. Assessing the limping child with skeletal scintigraphy. 39: 1056-1061
(2) J Nucl Med 1998; Mandell GA, et al. Bone scintigraphy in the detection of chronic recurrent multifocal osteomyelitis. 39: 1778-1783
(3) J Nucl Med 1996; Howarth DM, et al. Bone scintigraphy evaluated in diagnosing and staging Langerhans' cell histiocytosis and related disorders. 37(9):1456-60
(4) J Nucl Med 1994; Hardoff R, et al. Semiquantitative skull planar and SPECT bone scintigraphy in diabetic patients: differentiation of necrotizing (malignant) external otitis from severe external otitis. 35: 411-15
(5) Semin Nucl Med 1993; Sty JR, et al. Spine pain in children. 23: 296-320
(6) Radiology 1984; Strashum AM, et al. Malignant external otitis: Early scintigraphic detection. 150: 541-545
(7) Laryngoscope 1996; Stokkel MPM, et al. SPECT gallium scintigraphy in malignant external otitis: Initial staging and follow-up. Case reports. 106: 338-340
(8) J Nucl Med 2006; Frater C, et al. Bone scinitgraphy predicts outcome of steroid injection for plantar fasciitis. 47: 1577-1580
(9) Radiographics 2009; Khanna G, et al. Imaging of chronic recurrent multifocal osteomyelitis. 29: 1159-1177
(10) Radiology 2009; Fritz J, et al. Chronic recurrent multifocal
osteomyelitis: comparison of whole-body MR imaging with
radiography and
correlation with clinical and laboratory data. 252: 842-851
(11) Radiology 2012; Sweeney SA, et al. Case 181: synovitis acne
pustulosis hyperostosis osteitis (SAPHO) syndrome. 263: 613-617
(12) Radiographics 2013; Lew PP, et al. Imaging of disorders affecting the bone and skin. 34: 197-216