Two recent studies have taken a closer look at the role of gamma cameras and gamma probes in tracking the spread of breast cancer. In the first study, Japanese researchers compared SPECT to FDG-PET for detecting bone metastasis to the axial skeleton in breast cancer cases. In the second paper, French authors compared gamma probes for sentinel lymph node detection, which is an important guide for therapeutic choices.
Bone metastases
Up to 90% of patients with terminal distant breast cancer have bone metastasis, according to Dr. Takayoshi Uematsu and colleagues from Shizuoka Cancer Center Hospital in Shizuoka, Japan. As a result, imaging can assist in early detection before the development of significant neurologic and functional deficits.
"The spine is the most frequent site of cancer metastases; the posterior elements, including the pedicle, are the area of the vertebral body most frequently involved," they explained. "Breast cancer has a special predilection for the sternum that probably results from local spread from metastatic internal mammary nodes" (American Journal of Roentgenology, April 2005, Vol. 184:4, pp. 1266-1273).
While radionuclide bone scanning has been the gold standard for finding skeletal metastases, some reports have indicated that it is less effective than FDG-PET. On the other hand, FDG-PET may be less sensitive than SPECT imaging. Uematsu's group conducted their study to set the record straight.
Fifteen breast cancer patients underwent SPECT and FDG-PET scans within 49 days. The SPECT exam was done with a double-head gamma camera (e.cam, Siemens Medical Solutions, Erlangen, Germany), two to five hours after an injection of 740 MBq of 99mTc hydroxymethylene diphosphonate.
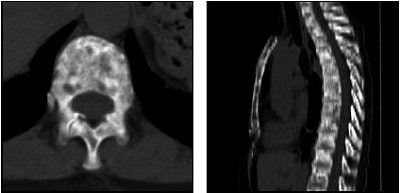 |
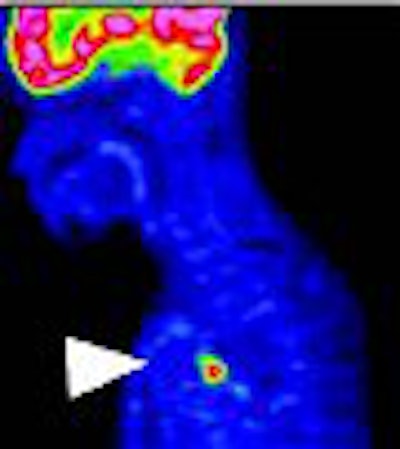
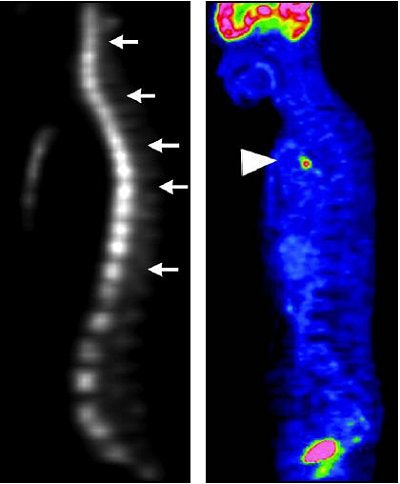
| A 63-year-old woman with osteoblastic bone metastases. Axial CT image (top left), 3D maximum-intensity-projection CT image (top right), sagittal SPECT image (bottom left), and sagittal FDG-PET image (bottom right) show osteoblastic deposits in vertebral bodies have increase in uptake of 99mTc hydroxymethylene diphosphonate (arrows), but not in uptake of FDG-PET. Hypermetabolic lesion in mediastinum (arrowhead) was confirmed to be lymph node recurrence. |
 |
| Uematsu T, Yuen S, Yuiksawa S, Aramaki T, Morimoto N, Endo M, Furukawa H, Uchida Y, Watanabe J, "Comparison of FDG PET and SPECT for Detection of Bone Metastases in Breast Cancer" (AJR 2005; 184:1266-1273). |
PET scans (Advance NXi, GE Healthcare, Chalfont St. Giles, U.K.) were started one hour after administration of 220-240 MBq of FDG. The authors pointed out that this FDG dose is lower than the norm, but more suitable for smaller Japanese patients. Finally, patients underwent CT and MRI scans to categorize metastases as osteolytic or osteoblastic.
According to the results, SPECT's sensitivity for diagnosing bone metastases was 85%, while the specificity was 99%. For FDG-PET, the sensitivity was 17% and the specificity was 100%. For metastasis classification, SPECT detected 92% of the 143 osteoblastic lesions and 35% of the 20 osteolytic sites. In comparison, FDG-PET found 6% of osteoblastic metastases and 90% of osteolytic ones.
"Bone SPECT altered patient treatment in one of the 15 patients.... Using FDG-PET, the bone metastasis was missed," the authors wrote. "The patient had a bone metastasis in the sternum."
SPECT is more accurate for differentiating benign and malignant lesions, the group concluded. However, FDG-PET is superior to SPECT for detecting osteolytic breast cancer metastases. They attributed this to technical differences in the two modalities -- SPECT is better for assessing bone destruction by tumor cells, while PET detects metabolic activity of tumor cells. Ultimately, they recommended that bone SPECT become routine in breast cancer tracking because of its high sensitivity.
ASLN detection
In a second study French investigators tested three gamma probes for sentinel lymph node detection in 200 breast cancer patients. The group's initial hypothesis was that the type of probe used did not affect axillary sentinel lymph node (ASLN) radiodetection, which turned out to be untrue.
"Axillary lymph node status currently remains one of the most important prognostic indicators in early breast cancer," wrote Dr. Jean-Marc Classe and colleagues. "The rate of ASLN detection depends not only on the skill and experience of the surgeon, but also on the performance of the gamma probe" (Journal of Nuclear Medicine, March 2005, Vol. 46:3, pp. 395-399).
Classe and many co-authors are from the René Gauducheau Cancer Center in Saint Herblain, France. Other contributors are from the Hospital and University Laennec in Saint Herblain and the Institut National de la Santé et de la Recherche Médicale in Nantes, France.
The following are the three probes used in this prospective study:
- Probe A: scintillator with bismuth germinate (BGO) crystal (Modelo 2, CEA/Damri, Gif-sur-Yvette Cedex, France)
- Probe B: semiconductor with cadmium telluride (CdTe) crystal (Navigator, Tyco Healthcare Group, Pembroke, Bermuda)
- Probe C: semiconductor with cadmium zinc telluride (CZT) crystal (Neoprobe, Neoprobe Corporation, Dublin, OH)
Unfiltered 99mTc-labeled rhenium sulfur colloids (Nanocis, CIS Bio International/Schering, Gif-sur-Yvette Cedex, France) were injected within the parenchyma of the tumor site. A positive finding of an ASLN was defined as the intraoperative detection of a number of counts per second that was at least twice the background level, the authors explained.
The majority of patients (45.5%) had a stage T1 tumor, and 37% of the tumor sites were in the external upper quadrant. The mean histologic size of the tumor was 12.14 mm, with a mean number of 9.3 nodes removed and a mean of 2.2 ASLN removed.
The mean ASLN activity was 52 kilobecquerel (kBq). While probes B and C were comparable for sensitivity, probe A performed much better -- sixfold higher than probe B or C when the injection was performed the morning of the operation and four times higher when performed the evening before.
Probe A's detection rate of 93% was also better than probe B at 86% and probe C at 90%. The false-negative rate for the three probes ranged from 20.7% to 22.2%, which was not deemed statistically significant.
Sensitivity is the main criterion when choosing a gamma probe, Classe's group concluded. Differences among probes could be an unrecognized cause of different success rates for ASLN detection, they added.
"This is an important consideration, as detection failure implies that the patient will undergo axillary resection and thereby have a lower quality of life than will a patient undergoing only ASLN excision," they stated.
By Shalmali Pal
AuntMinnie.com staff writer
April 29, 2005
Related Reading
PEM development picks up pace, February 7, 2005
15O-water PET shows persistence of blood flow in chemo-resistant breast tumors, November 28, 2003
Copyright © 2005 AuntMinnie.com




















