European researchers have developed a way to use FDG-PET to measure glucose metabolism in patients with severe brain injuries to diagnose and predict when they will recover consciousness, according to a study published online on 26 May in Current Biology.
Using data from FDG-PET images, the researchers found patients with glucose metabolism below 42% of normal cortical brain activity appeared to be fully unconscious and did not recover from that state at one-year follow-up. By comparison, individuals above that 42% threshold exhibited signs of awareness during an initial exam or had recovered consciousness within one year.
"The method is objective and computationally simple and provides easily interpretable results," wrote lead author Dr. Johan Stender and colleagues from the University of Copenhagen in Denmark and the University of Liège in Belgium. "Overall, this represents an important improvement to current nonquantitative diagnostic approaches with FDG-PET."
Challenging assessment
Stender and colleagues noted in the study one challenge facing clinicians is accurately differentiating between a patient in a minimally conscious state and a person who has unresponsive wakefulness syndrome, because some brain injury patients can maintain certain levels of awareness despite appearing fully unresponsive.
Clinically speaking, a person in a minimally conscious state sometimes will respond to sounds or other stimuli and is not in such a deep state of unconsciousness that he or she is in a coma. Unresponsive wakefulness syndrome, previously known as a vegetative state, is more severe; patients are totally unaware of themselves or their surroundings.
While previous studies have proposed FDG-PET as one method to evaluate the cerebral metabolic rate of glucose to assess consciousness, "current methods are nonquantitative and have important drawbacks deriving from visually guided assessment of relative changes in brain metabolism," the authors wrote.
Thus Stender and colleagues explored the possibility of developing more reliable diagnostic markers to assess current and future levels of consciousness when clinically evaluating a patient at bedside.
Researchers used FDG-PET to image and map cerebral glucose metabolism in 131 brain-injured patients suffering from either full or partial loss of consciousness and 28 healthy control subjects. By analyzing FDG-PET data, the goal was to establish an optimum glucose metabolism rate for cortical tissue -- which the authors called the cortical metabolic index -- to use as a diagnostic marker to predict which patients would recover.
Glucose parameters
Researchers decided to measure cortical metabolic index in the least-injured cortical hemisphere, because there is evidence that only one brain hemisphere is necessary for conscious awareness.
As one might expect, FDG-PET data recorded a higher mean cortical metabolic index in healthy subjects (7.59 ± 1.19), compared with patients with unresponsive wakefulness syndrome (2.88 ± 0.74; 38% of normal activity) and patients in a minimally conscious state (4.23 ± 1.03, 56% of normal). Among patients in a minimally conscious state who eventually emerged from their condition, the mean cortical metabolic index was 4.76 ± 0.65, or 63% of normal activity.
| Cortical metabolic index levels based on FDG-PET scans | ||||
| Healthy subjects | Unresponsive wakefulness syndrome | Minimally conscious state -- all patients | Minimally conscious state patients who recovered | |
| Mean cortical metabolic | 7.59 ± 1.19 | 2.88 ± 0.74 | 4.23 ± 1.03 | 4.76 ± 0.65 |
| Percent of normal | 100% | 38% | 56% | 63% |
Researchers measured the effectiveness of setting a specific cortical metabolic index level in predicting which consciousness category patients fell into -- unresponsive wakefulness or minimally conscious state -- using receiver operator characteristic (ROC) analysis to calculate an area under the curve (AUC) value. Using an index of 3.19 (42% of normal activity) offered the best classification, with an 88% correct classification, sensitivity of 95%, and specificity of 78%.
Patient outcomes
To determine eventual outcome, researchers gathered data from 119 (91%) patients at the one-year follow-up. Again, using the metabolic index threshold of 42%, the study correctly predicted 88% of all known patient outcomes, with 95% sensitivity and 76% specificity at follow-up.
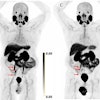
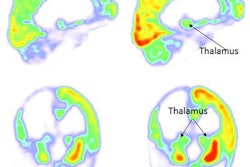
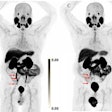
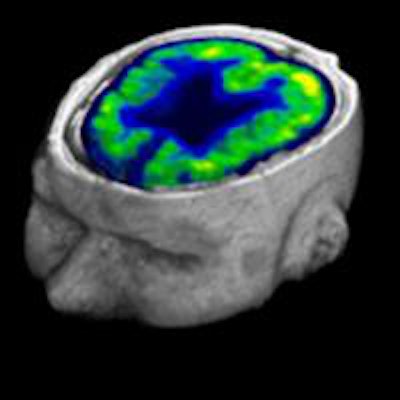
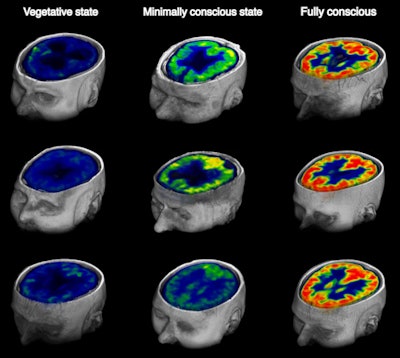 Images show brain glucose metabolism as seen on FDG-PET at rest in patients with chronic disorders of consciousness and fully conscious control subjects. There is a significant reduction in brain glucose metabolism from full consciousness to the minimally conscious state and unresponsive wakefulness syndrome. Images courtesy of Stender et al.
Images show brain glucose metabolism as seen on FDG-PET at rest in patients with chronic disorders of consciousness and fully conscious control subjects. There is a significant reduction in brain glucose metabolism from full consciousness to the minimally conscious state and unresponsive wakefulness syndrome. Images courtesy of Stender et al.There were 11 unresponsive wakefulness syndrome patients with a brain metabolism activity above the 42% diagnostic threshold. Of those 11 cases, eight people (72%) regained consciousness after one year, while the other three people died during that time.
There were three minimally conscious state patients who were below the diagnostic 42% metabolism benchmark. One person died, one patient had no change in clinical condition, and one individual was lost to follow-up.
Stender and colleagues concluded the findings suggest the brain undergoes a fundamental change at a certain level of metabolism, or energy, which activates the brain when it reaches that threshold. At that point of energy, the patient has a greater chance of regaining consciousness.
"The threshold of 42% of normal cortical hemispheric metabolic activity represents the minimal energetic requirement predictive of regaining consciousness," the authors wrote. "FDG-PET thus constitutes a strong diagnostic and prognostic marker in [disorders of consciousness] arising from brain injury, irrespective of its pathogenesis."
The Danish and Belgian researchers added their findings also provide direction for future research.