PET/MRI imaging with an experimental prostate-specific membrane antigen (PSMA) radiotracer appears superior to biparametric MRI alone for diagnosing primary prostate cancer, according to a study published March 28 in Prostate International.
Chinese researchers compared results of the two approaches -- either PET/MRI imaging with the tracer F-18 PSMA-1007 or biparametric MRI (bpMRI) -- for diagnosing primary prostate cancer in patients with suspected tumors. By all measures, including sensitivity and specificity, PET/MRI performed better, the authors wrote.
"The diagnostic value of F-18 PSMA-1007-PET/MRI for the detection of [prostate cancer] is better than that of bpMRI," wrote corresponding author Guihua Jiang, PhD, of Guangdong Second Provincial General Hospital in China.
Biparametric MRI (bpMRI) imaging of the prostate is itself a relatively new approach. The method combines both morphologic T2-weighted imaging (T2WI) and diffusion-weighted imaging (DWI), and it is emerging as an alternative to multiparametric MRI (mpMRI), given that mpMRI involves the use of contrast agents with known side effects.
Moreover, although mpMRI and bpMRI have been introduced as novel imaging approaches for diagnosis and localization of primary prostate lesions, as well as guiding prostate biopsy, they have poor detection rates of low-grade disease, which can result in missed diagnoses, the authors wrote.
Conversely, hybrid PET/MRI imaging provides diagnostic information at a molecular level, much earlier in the development of the disease. Radiotracers such as F-18 PSMA-1007 are designed to detect overexpressed PSMA on cancer cells, and clinical evidence is growing in support of this approach.
In this study, Jiang and colleagues aimed to add to this body of evidence by analyzing F-18 PSMA-1007 PET/MRI results in a head-to-head comparison with bpMRI.
The researchers looked at imaging of 29 consecutive male patients with suspected prostate cancer who underwent preoperative whole-body F-18 PSMA-1007-PET/MRI scans (3-tesla Biograph mMR, Siemens Healthineers), and subsequent targeted biopsy for suspected cancerous lesions (n = 48) between June 2019 and June 2021.
Two nuclear medicine physicians with more than five years of experience each interpreted the images. First, they assessed all bpMRI images of each suspected lesion. Next, they studied the PET images with the MRI images as anatomical background. Finally, they reviewed all lesions with access to the individual evaluations of PET and bpMRI images to arrive at combined PET/MRI findings.
In addition, the group studied whether the PET/MRI and bpMRI results correlated with International Society of Urological Pathology (ISUP) grades, an effective new clinical cancer severity grading system. These correlations were based on receiver operating characteristic (ROC) curves of optimal standardized uptake values (SUVmax) for PET/MRI and apparent diffusion coefficients (ADC) for bpMRI.
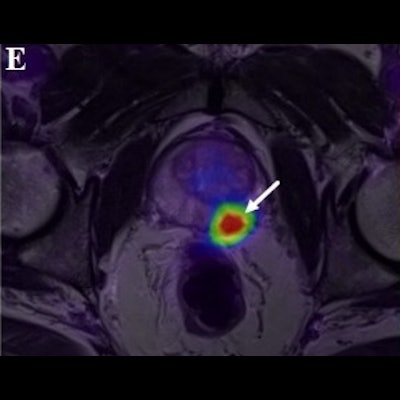
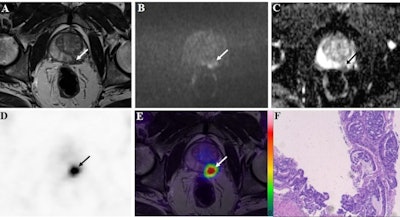 A 72-year-old patient with a prostate-specific antigen (PSA) level of 50.8 ng/ml. The lesion with tumor diameter of 11.7 mm (arrow) was evaluated as positive (PI-RADS score 4) on bpMRI with T2WI image (A), DWI image (B), and ADC map (C), indicating prostate cancer lesion. On F-18 PSMA-1007 PET image (D), the lesion showed intense uptake with an SUVmax of 79.6 (PSMA-RADS score 5). Combined with bpMRI and PET score, fused F-18 PSMA-1007 PET/MRI image (E) further suggested prostate cancer. Subsequent biopsy results (F) proved prostate cancer lesion of ISUP grade 5 with Gleason score 5+4. Image courtesy of Prostate International.
A 72-year-old patient with a prostate-specific antigen (PSA) level of 50.8 ng/ml. The lesion with tumor diameter of 11.7 mm (arrow) was evaluated as positive (PI-RADS score 4) on bpMRI with T2WI image (A), DWI image (B), and ADC map (C), indicating prostate cancer lesion. On F-18 PSMA-1007 PET image (D), the lesion showed intense uptake with an SUVmax of 79.6 (PSMA-RADS score 5). Combined with bpMRI and PET score, fused F-18 PSMA-1007 PET/MRI image (E) further suggested prostate cancer. Subsequent biopsy results (F) proved prostate cancer lesion of ISUP grade 5 with Gleason score 5+4. Image courtesy of Prostate International.Out of the 48 suspected prostate cancer lesions in 29 patients, 38 were identified with biopsies as clinically significant prostate cancer, and 10 were noncancerous lesions. Against these pathological results, F-18 PSMA-1007 PET/MRI demonstrated much greater diagnostic accuracy (area under the curve [AUC]), sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) than bpMRI, the researchers found.
| Diagnostic accuracy of bpMRI and F-18 PSMA-1007 PET/MRI for detecting prostate cancer | ||
| bpMRI | F-18 PSMA-1007 PET/MRI | |
| Sensitivity | 92.11% | 94.7% |
| Specificity | 50% | 100% |
| PPV | 87.50% | 100% |
| NPV | 62.50% | 83.33% |
| AUC | 0.711 | 0.974 |
| p-value | 0.0029 | |
In addition, a high SUVmax of F-18 PSMA-1007 radiotracer detected on PET/MRI may indicate a lesion with a high ISUP grade, the authors wrote. The semiquantitative parameters of SUVmax demonstrated a higher AUC (0.874) than that of ADC (0.776) for detecting prostate cancer.
"F-18 PSMA-1007 PET/MRI has a greater diagnostic value for detecting [prostate cancer] than bpMRI, and SUVmax shows a good correlation with the ISUP grade," the researchers wrote.
The authors noted limitations, namely that this was a retrospective, single-center study with a relatively small number of patients. Also, as yet, there is no standardized clinical scoring system available for detecting prostate cancer lesions using bpMRI or F-18 PSMA-1007 PET/MRI, as both are new approaches.
Nevertheless, the study shows a high diagnostic value of F-18 PSMA-1007 PET/MRI and revealed associations between SUVmax values and ISUP grades for prostate cancer, which is a step in that direction, they wrote.
"Our study may provide a reference for the clinical applications of F-18 PSMA-1007 PET/MRI and enrich the literature," Jiang and colleagues concluded.