A patient’s body mass index (BMI) has a significant effect on how much radiation exposure they receive from chest imaging in cases of suspected cardiac ischemia, according to a study published April 9 in the Journal of the American Heart Association.
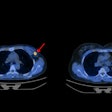
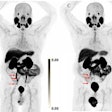
Cardiologists at Saint Luke's Mid America Heart Institute in Kansas City, MO, found that as BMI increases, so too does radiation exposure, although PET offers the least variability, followed by SPECT, and then coronary CT angiography (CCTA). The finding is key to providing “patient-centered” care, the group wrote.
“These data may be helpful to generate more accurate estimations of radiation effective dose by BMI for each imaging modality and are important for making patient‐centered decisions for ischemic testing,” noted lead author Brett Sperry, MD, and colleagues.
Heavier patients tend to have greater “attenuation” -- a reduction of the radiation signal as it passes through tissue -- because of increased tissue density and thickness. Thus, more radiation is required to produce clear images, the authors explained. While knowledge of differences in radiation effective dose to patients with chest pain across imaging modalities is essential to a patient‐centered approach, BMI is an “important and underappreciated” predictor of effective dose, they added.
To address this knowledge gap, the group analyzed radiation exposure based on BMI in patients who underwent PET/CT, SPECT/CT, and CCTA for suspected cardiac ischemia, which causes chest pain due to a lack of blood flow from the coronary arteries to the heart.
All imaging was performed on state-of-the-art scanners using optimal radiation‐sparing protocols, the authors noted. Among 9,046 patients with a mean BMI of 30.6 kilograms per square meter (kg/m2), 4,787 were imaged with PET/CT, 3,092 were imaged with SPECT/CT, and 1,167 were imaged with CCTA.
According to the analysis, median radiation effective doses were 4.4 mSv for PET/CT, 4.9 mSv for SPECT/CT, and 6.9 mSv for CCTA. Patients at a BMI < 20 kg/m2 had similar radiation effective dose with all three imaging modalities, while those with BMI ≥ 20 kg/m2 had the lowest effective dose with PET/CT, the group found.
Moreover, radiation effective dose and variability increased dramatically with CCTA as BMI increased, and was 10 times higher in patients with BMI > 45 kg/m2 compared with < 20 kg/m2 (median, 26.9 vs. 2.6 mSv), the group noted.
“Although median radiation exposure is modest across state‐of‐the‐art PET/CT, SPECT/CT, and CCTA systems using optimal radiation‐sparing protocols, there are significant variations across modalities based on BMI,” the group wrote.
The authors noted that 2021 multisocietal chest pain guidelines and 2023 appropriate use criteria recommend either CCTA or nuclear stress testing as first‐line imaging modalities in the evaluation of chest pain as well as advocate for a patient‐centered imaging strategy.
To that end, they suggested that choosing an imaging approach based on patient BMI may lead to lower radiation effective dose when imaging for chest pain.
“These data are important for making patient‐centered decisions for ischemic testing,” the group concluded.
The full study is available here.