VIENNA - Hybrid imaging is gaining acceptance as opportunities using combinations of modalities emerge and promise to optimize cardiac imaging, according to expert speakers in today's session called "Hybrid cardiovascular imaging: Where should we go?"
Not only is SPECT a widely available and very effective method for perfusion imaging, but also functional imaging with SPECT or PET is necessary to exclude coronary artery disease (CAD), as the positive predictive value of CT for relevant stenoses is very limited, noted Dr. Marcus Hacker, a specialist in cardiac imaging from the Medical University of Vienna. In his talk today entitled "SPECT/CT: Is it just PET/CT's little brother?" he plans to discuss the pros and cons of the two combined modes of imaging.
Appropriate diagnosis and therapy of CAD frequently require information about both the morphological and functional status of the coronary artery tree. With this in mind, combined imaging consisting of invasive coronary angiography (ICA) plus SPECT myocardial perfusion imaging (MPI) is being used for the clinical diagnosis of patients with stable angina. However, knowledge regarding the presence and extent of subclinical coronary atherosclerosis in patients who do not have ischemia by MPI can be of importance in patient management, and, for this reason, PET might be preferable to SPECT for providing the necessary information for diagnosis and prognosis.
During his presentation, Hacker will explain why this is the case. His focus will mainly be on different strategies to combine SPECT functional and perfusion imaging with different CT techniques on SPECT/CT hybrid scanners, but also by the use of separate SPECT and CT scanners. He will also discuss the advantages of PET/CT.
"In general, ICA is an invasive method with a low but distinct rate of complications. For the purpose of coronary diagnosis, ICA is two-dimensional and with it, pathologies can only be virtually combined with perfusion abnormalities in SPECT, so that the allocation is hampered particularly in patients with multivessel or multistenotic disease," he stated.
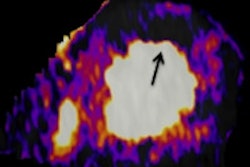
As an alternative, PET/CT as compared to SPECT/CT provides higher spatial resolution and absolute quantification of perfusion so that higher accuracy can be achieved, Hacker pointed out. "Otherwise, with SPECT strategies, more physiological ergometric or treadmill stress tests can be performed, and perfusion tracers are more widely available."
However, he highlighted that the combination of noninvasive CT angiography with SPECT was advantageous as both modalities provided 3D images that can be fused. "This results in improved allocation from vessels and stenoses to respective ischemia and, thus, reduces the number of ambiguous findings," he said, adding that wall irregularities as well as noncalcified plaque tissue were detectable from CT, and improved SPECT risk stratification. "This kind of image fusion can be generated from both standalone and hybrid scanners."
But Hacker emphasized that the hemodynamic relevance of coronary artery lesions is a major condition to decide whether an interventional therapy should be performed or not. "Identifying morphologically significant stenoses in CT coronary angiography does not mean that these stenoses are hemodynamically significant or that these stenoses required interventional therapy," he commented. "Functional imaging is mandatory in patients with these kinds of stenoses, and, in addition, SPECT provides useful information for both risk stratification and patient management for patients with stenoses or even increased calcium scores."
SPECT accuracy and risk stratification are based on a huge amount of published registry data and prospective trials, and SPECT can be performed in nearly every patient in good quality, according to Hacker. Furthermore, SPECT quantification has been established for many years, and published quantitative values exist to enable valid patient selection for interventional therapy and risk stratification.
"These are clear advantages over all concurring methods in perfusion imaging. In combination with SPECT, CT enables absolute flow quantification compared to SPECT, and can be balanced as multivessel disease can be easily identified from CT," he remarked.
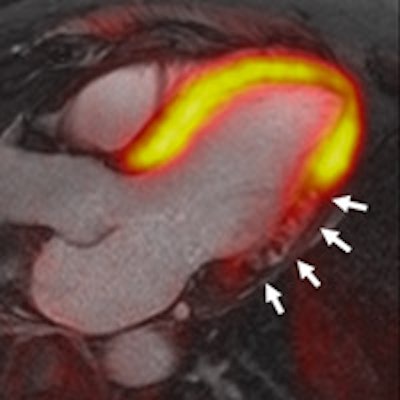
Also speaking in the same session, giving a talk entitled "MR/PET: Do we really need it?" Prof. Harald Quick will address PET/MR. In 2010 and 2011, the first whole-body PET/MR systems, sequential and simultaneous, respectively, became available. "With PET/MR we are still in an early phase of clinical application," he said. "While the focus initially was on oncologic whole-body PET/MR, we are now seeing the first cardiovascular applications."
The introduction of PET/MR and its potential use as a cardiac hybrid imaging modality was essential for the technical and physical integration of a PET detector within a whole-body MR system. Quick, who was recently appointed director of the Erwin L. Hahn Institute for MRI and head of high-field and hybrid MRI in Essen, Germany, explained how this integration allowed for independent and simultaneous PET and MR data acquisition, adding that simultaneous hybrid data acquisition not only saves examination time when compared with two independent examinations but also provides the potential to perform motion correction of the hybrid imaging data.
MRI provides excellent soft-tissue contrast, quantification of cardiac function and blood flow, as well dynamic perfusion imaging, and can be considered as the gold standard for many cardiac imaging applications. "In combination with PET, this may improve the assessment of myocardial viability and myocarditis, to name only two examples," he said.
However, PET/MR is still a relatively new introduction to hybrid imaging, and existing limitations are the subject of ongoing research. Notably, MR-based attenuation correction (AC) of PET data is an active field of research in PET/MR. "Attenuation correction in PET imaging is a precondition to obtain quantitative data about the metabolism of the radiotracer in different tissues, for example, the myocardium and/or lesions. In PET/MR, AC has to be performed in a fundamentally different way than AC in PET/CT, where the attenuation data is obtained by a CT scan," he noted.
Addressing the question posed in the title of his talk, Quick said that it was still very early to answer this question, and that cardiovascular PET/MR has just been realized in a clinical setting and only future years of research and a broader clinical application would provide the answer. However, considering the technique's large inherent clinical potential, the fact that MRI is already the gold standard for numerous cardiovascular imaging indications, and the simultaneous combination with metabolic information from PET, in his opinion, the answer is most likely to be "yes."
Originally published in ECR Today on 6 March 2014.
Copyright © 2014 European Society of Radiology